6 Oct 2025
- 20 Comments
Acid Reflux Symptom Checker
Answer the questions below to help determine if your symptoms might indicate acid reflux or LPR (silent reflux). This tool is educational and not a substitute for medical advice.
Your symptom analysis will appear here after clicking "Analyze My Symptoms"
Common Trigger Foods to Avoid:
Did you know that up to half of people who complain of a chronic sore throat actually have hidden acid reflux? It’s not a coincidence - the acid that climbs up from the stomach can irritate the same tissues that make up your voice box and throat. This article unpacks why that happens, how to tell the difference, and what simple steps can ease both problems.
Key Takeaways
- Acid reflux can cause a sore throat through a condition called laryngopharyngeal reflux (LPR).
- Typical reflux symptoms like heartburn may be absent, making diagnosis tricky.
- Diet, weight, and bedtime habits are the biggest controllable triggers.
- Over‑the‑counter antacids work for occasional flare‑ups, but proton pump inhibitors are often needed for chronic cases.
- Seek medical advice if the sore throat lasts more than three weeks or you notice breathing or swallowing difficulties.
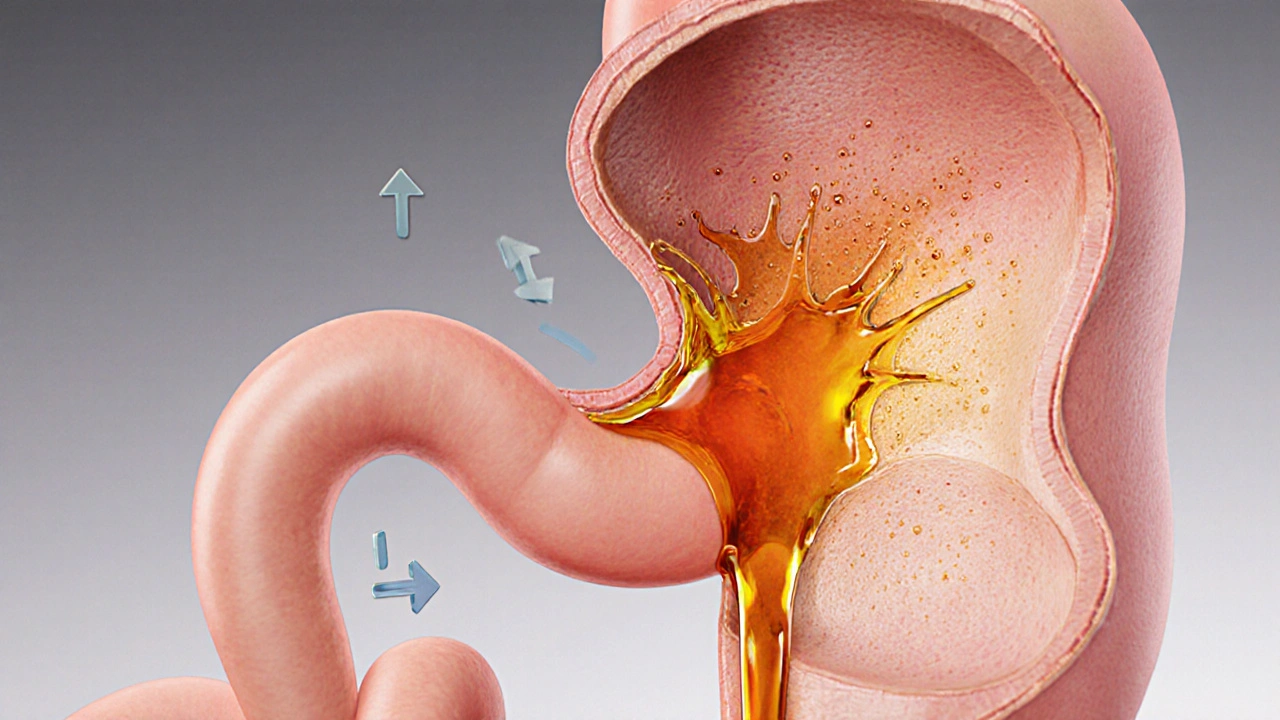
What Is Acid Reflux?
Acid reflux is the backflow of stomach acid into the esophagus, the tube that connects your mouth to your stomach. When the lower esophageal sphincter (LES) - a ring of muscle at the bottom of the esophagus - doesn’t close tightly, acid can splash up, creating a burning sensation called heartburn. While many people experience occasional heartburn after a big meal, frequent episodes point to gastroesophageal reflux disease (GERD), a chronic condition that may damage the esophageal lining.
Why a Sore Throat Shows Up
Sore throat is pain, scratchiness, or irritation in the throat that worsens when you swallow. Most of us think of colds, strep infections, or allergies, but reflux‑related irritation is a silent contributor. When acid reaches the larynx (voice box) and pharynx (throat), it can inflame the delicate mucous membranes, leading to a raw feeling, hoarseness, or a persistent cough.

Laryngopharyngeal Reflux (LPR): The Hidden Link
Laryngopharyngeal reflux (LPR) is a form of reflux where stomach contents travel past the esophagus and irritate the throat and voice box. Unlike typical GERD, LPR often occurs without the classic heartburn, earning it the nickname “silent reflux.” The acid can sit on the throat tissues for hours, especially when you lie down, causing chronic hoarseness, a feeling of a lump in the throat (globus), or frequent throat clearing.
Spotting the Overlap: Symptoms to Watch
- Morning hoarseness or a raspy voice that improves during the day.
- A persistent sore throat that doesn’t respond to lozenges.
- Frequent throat clearing or a sensation of mucus buildup.
- Dry cough, especially after meals or at night.
- Heartburn, sour taste, or belching - but these may be mild or absent in LPR.
If you notice several of these signs together, consider reflux as a possible cause.
Everyday Triggers You Can Tame
Identifying and adjusting lifestyle factors often provides the quickest relief.
- Watch your meals. Large, fatty, or spicy meals relax the LES. Aim for smaller portions and limit fried foods, chocolate, citrus, and tomato‑based sauces.
- Mind the timing. Avoid eating within three hours of bedtime. Lying down makes it easier for acid to travel upward.
- Elevate the head of your bed. Raising the mattress 6-8 inches uses gravity to keep stomach contents down.
- Weight management. Extra abdominal pressure from obesity can push acid up. Even a modest 5‑10% weight loss can improve symptoms.
- Quit smoking and limit alcohol. Both weaken the LES and increase acid production.
- Stay hydrated. Water helps dilute stomach acid and clears mucus from the throat.
Medications: From Antacids to PPIs
When lifestyle tweaks aren’t enough, medicines step in.
- Antacids are quick‑acting tablets that neutralize stomach acid. They’re great for occasional flare‑ups but don’t heal underlying damage. \n
- H2‑blockers (e.g., ranitidine, famotidine) reduce acid production for a longer period than antacids. Effects last 8‑12hours.
- Proton pump inhibitors (PPIs) (e.g., omeprazole, esomeprazole) block the final step of acid secretion, providing the strongest relief. They’re the go‑to for chronic GERD or LPR, often taken once daily before breakfast.
Long‑term PPI use should be monitored by a doctor because it can affect calcium absorption and increase infection risk.

When to See a Healthcare Professional
If any of the following apply, schedule an appointment:
- Sore throat lasts longer than three weeks.
- Difficulty swallowing, breathing, or a persistent lump‑like feeling in the throat.
- Frequent nighttime coughing or choking.
- Weight loss or loss of appetite.
- Symptoms persist despite over‑the‑counter medication and lifestyle changes.
A doctor may order an upper endoscopy, pH monitoring, or a laryngoscopic exam to confirm reflux and rule out other conditions.
GERD vs. LPR: Quick Comparison
| Aspect | GERD | LPR (Silent Reflux) |
|---|---|---|
| Typical symptom | Heartburn, regurgitation | Hoarseness, chronic sore throat, globus |
| Acid location | Esophagus | Throat & voice box |
| Often present | Yes | No classic heartburn (can be absent) |
| Diagnostic test | Upper endoscopy, esophageal pH test | 24‑hour dual‑probe pH monitoring |
| First‑line treatment | Lifestyle changes + antacids/H2‑blockers | Lifestyle changes + PPIs (often higher dose) |
Bottom Line
Understanding that a sore throat can be a warning sign of acid reflux opens the door to effective relief. By spotting the pattern, adjusting daily habits, and using the right medication when needed, most people can quiet the irritation and protect their throat long‑term. Remember, if symptoms linger or worsen, a professional evaluation is the safest next step.
Frequently Asked Questions
Can I have acid reflux without heartburn?
Yes. Laryngopharyngeal reflux often presents without the classic burning sensation, showing up instead as a sore throat, hoarseness, or chronic coughing.
How long does it take for lifestyle changes to improve my throat?
Most people notice a reduction in irritation within one to two weeks of consistent changes, such as eating smaller meals, avoiding trigger foods, and elevating the head of the bed.
Are over‑the‑counter antacids enough for chronic sore throat?
Antacids can relieve occasional flare‑ups, but chronic symptoms usually need stronger therapy like an H2‑blocker or a proton pump inhibitor prescribed by a doctor.
What foods should I avoid if I suspect reflux?
Common triggers include fried foods, chocolate, peppermint, citrus fruits, tomatoes, coffee, and carbonated drinks. Keeping a food diary helps pinpoint personal triggers.
When is it necessary to get an endoscopy?
If you have alarm symptoms-such as difficulty swallowing, unexplained weight loss, bleeding, or persistent pain-an upper endoscopy helps assess damage and rule out other conditions.

Kimberly :)
October 6, 2025Interesting take on reflux, but I think many readers overlook the role of stress hormones 🧠. While diet is crucial, cortisol spikes can relax the LES as well. 🍋💪
Sebastian Miles
October 10, 2025From a clinical standpoint, the pathophysiology involves transient LES relaxations – that’s the key mechanism.
Harshal Sanghavi
October 13, 2025Sure, because ignoring the obvious always solved problems, right? But hey, if you love the chronic cough, keep doing what you’re doing.
Duke Gavrilovic
October 16, 2025One must acknowledge that lifestyle modification is the cornerstone of therapy. Nevertheless, the evidence supporting PPIs in LPR remains somewhat equivocal. Accordingly, a judicious trial is advisable.
Abby VanSickle
October 20, 2025While I appreciate the thoroughness, the article downplays the urgency of persistent throat pain. Ignoring alarm symptoms is simply negligent, and it undermines patient safety.
chris macdaddy
October 23, 2025hey guys, these tips r good but pls try not to eat late. i found that even a little snack before bed can cause a whole night of cough. just a thought!
Moumita Bhaumik
October 27, 2025Do you really think it’s just a "diet issue"? Wake up! Big pharma wants you to swallow pills forever while they hide the real cause – engineered food additives that erode the esophageal lining.
Sheila Hood
October 30, 2025Antacids are just placebo sugar.
Melissa Jansson
November 3, 2025Let’s not forget that the culinary world is a minefield of hidden reflux triggers. Even “healthy” smoothies can be acid‑laden if you blend citrus with almond milk. The reality is far more nuanced than the article suggests.
Max Rogers
November 6, 2025Great summary! I’d add that tracking symptoms in a journal can help pinpoint personal triggers more accurately.
Louie Hadley
November 10, 2025Appreciate the balanced view. It’s important to remember that each body reacts differently, so a one‑size‑fits‑all approach rarely works.
Ginny Gladish
November 13, 2025The article is riddled with oversimplifications. First, it treats GERD and LPR as if they’re interchangeable, which is medically inaccurate. Second, it glosses over the potential side effects of long‑term PPI use. Finally, the recommended lifestyle changes are presented as a panacea, ignoring socioeconomic barriers that many patients face.
Faye Bormann
November 17, 2025When I first read the piece, I was struck by how it veers away from mainstream medical narratives, daring to suggest that the “standard diet” may be the silent accomplice to our discomfort. The author argues that the typical Western breakfast-rich in processed sugars and low‑fat dairy-creates a cascade of hormonal imbalances that predispose the lower esophageal sphincter to premature relaxation. Moreover, the piece highlights the often‑ignored role of gut microbiota, noting that dysbiosis can amplify inflammatory pathways, leading to heightened acid production. It then delves into the concept of “chronobiological eating,” which posits that aligning meals with circadian rhythms can reduce nocturnal reflux episodes; this is supported by emerging research from gastroenterology labs. The discussion of “micro‑pricks”-tiny, recurrent bouts of acid exposure that don’t trigger overt heartburn-sheds light on why many patients experience chronic throat irritation without classic GERD symptoms. The author also critiques the overreliance on proton pump inhibitors, warning of potential nutrient malabsorption and increased infection risk, urging clinicians to prioritize lifestyle first. In addition, the article suggests that modest weight loss-just five percent of body weight-can dramatically improve LES tone, a point often underemphasized in conventional advice. It recommends a stepped approach: begin with dietary elimination (cutting fried foods, chocolate, caffeine, and carbonated beverages), then incorporate positional therapy by elevating the head of the bed by six to eight inches. Finally, the piece acknowledges the psychosocial component: chronic stress can amplify reflux via heightened cortisol, thus recommending mindfulness practices. Overall, the article weaves together clinical data, emerging science, and practical suggestions, offering a comprehensive roadmap for anyone grappling with the elusive link between acid reflux and a stubborn sore throat.
Kathy Butterfield
November 20, 2025Loving the practical tips! 😊👍 Elevating the bed and cutting out soda are game‑changers. 🙌
Zane Nelson
November 24, 2025While the author’s enthusiasm is evident, the prose suffers from an overabundance of platitudinous phrasing, rendering the content superficial rather than insightful. A more rigorous engagement with primary literature would have elevated the discussion.
Sahithi Bhasyam
November 27, 2025Great article!! I think it really covers a lot...but maybe add more about how spices affect us?? Thnx! :)
mike putty
December 1, 2025Stay hopeful! Small changes often lead to big improvements in throat comfort.
Kayla Reeves
December 4, 2025We must not normalize self‑medication; people need to understand the moral responsibility of seeking professional care.
Abhinanda Mallick
December 8, 2025It’s absurd that Western diets continue to dominate global cuisine while they poison our throats. True health comes from respecting traditional, low‑acid foods, not from chasing cheap, processed fare that the global elite push.
Richard Wieland
December 11, 2025In essence, mindful eating may bridge the gap between symptom and solution.