19 Nov 2025
- 12 Comments
Every year, millions of people take prescription drugs, over-the-counter medicines, and dietary supplements without issue. But for some, a medication that works for others can cause serious harm. Maybe it’s an unexpected rash, a sudden drop in blood pressure, or a strange reaction that doesn’t show up on the label. When that happens, reporting it isn’t just helpful-it’s critical. The FDA’s MedWatch program exists for exactly this reason: to catch safety problems that clinical trials miss.
What Is MedWatch, Really?
MedWatch is the U.S. Food and Drug Administration’s official system for collecting reports about harmful side effects from drugs, medical devices, dietary supplements, and even some foods and cosmetics. It’s not a fancy app or a high-tech AI tool. It’s a simple, human-driven reporting system that’s been running since 1993. And despite its low-tech appearance, it’s one of the most important safety nets in American healthcare.The FDA doesn’t test every drug on every person before it hits the market. Clinical trials involve thousands, not millions. That means rare side effects-like one in 10,000 people-can slip through. MedWatch fills that gap. When a doctor, pharmacist, patient, or caregiver notices something unusual, they can report it. These reports pile up, and when enough people report the same problem, the FDA takes notice.
Think of MedWatch like a smoke alarm. It doesn’t tell you what’s burning, but it alerts you that something’s wrong. That’s why even if you’re not 100% sure a drug caused the reaction, you should still report it. The FDA doesn’t need proof-they need signals.
Who Can Report to MedWatch?
Anyone can report. That includes:- Healthcare professionals (doctors, nurses, pharmacists)
- Patients and family members
- Pharmaceutical companies (they’re legally required to)
- Hospitals and medical device facilities
But here’s the truth: most reports come from manufacturers. About 85% of the 1.3 million reports the FDA gets each year are from drug companies. That leaves only 15% from doctors and patients. And that’s a problem.
Studies show only about 6% of serious adverse reactions are ever reported. Why? Because many healthcare providers don’t know how, don’t have time, or think it’s not their job. Patients often don’t realize they can report at all.
What Counts as a Reportable Event?
Not every minor side effect needs a report. The FDA defines a serious adverse event as one that:- Results in death
- Requires hospitalization
- Causes permanent disability
- Leads to a birth defect
- Is life-threatening
- Requires medical or surgical intervention to prevent one of the above
Even if the reaction isn’t listed on the drug label, report it. If you’re unsure whether it’s serious, err on the side of caution. The FDA says: “If you’re not sure, report it anyway.”
Examples:
- After taking a new blood pressure med, you develop severe swelling in your throat and need emergency care.
- Your elderly parent starts having seizures after starting a new antidepressant.
- A child develops a rare skin rash after taking a common OTC cold medicine.
These are all reportable-even if the drug is FDA-approved and widely used.
How to Report: The Three Forms
There are three forms, depending on who’s reporting:- FDA Form 3500 - For healthcare professionals. This is the most detailed version. It asks for patient info (without names), drug name and dosage, when the reaction happened, symptoms, lab results, and what was done to treat it.
- FDA Form 3500B - For patients and consumers. This one uses plain language. No medical jargon. It’s available in English and Spanish. Takes about 15-20 minutes to fill out.
- FDA Form 3500A - For manufacturers and hospitals. This is mandatory. Companies must report serious events within 15 days.
You can find all forms on the FDA MedWatch website. You can download, print, and mail them-or fill them out online. The online version is faster and includes helpful drop-down menus.
For patients: You don’t need a doctor’s note. You don’t need medical records. Just answer the questions as best you can. If you don’t know the exact dose or date, write “unknown.” The FDA knows you’re not a clinician.
What Happens After You Report?
You might never hear back. And that’s normal.Less than 15% of reporters get any follow-up. That doesn’t mean your report didn’t matter. It means the system is overwhelmed. The FDA receives over a million reports a year. They can’t reply to each one.
But here’s what actually happens:
- Your report gets added to the FDA Adverse Event Reporting System (FAERS), a massive database.
- Analysts look for patterns-like 20 different people reporting the same rare liver injury after taking Drug X.
- If a pattern emerges, the FDA may launch a formal study, update the drug label, or even issue a warning or recall.
Some of the most important drug safety actions in the last 20 years started with a single MedWatch report. The withdrawal of Vioxx (a painkiller) after heart risks emerged? It began with scattered reports from patients and doctors.
Why Don’t More People Report?
A 2023 survey of 1,200 U.S. physicians found that 68% rarely or never report adverse events. Why?- Time - Filling out the form takes 12-20 minutes. In a busy clinic, that’s hard to squeeze in.
- Doubt - “Was it really the drug? Maybe it was something else.”
- Confusion - “I thought only manufacturers had to report.”
- No feedback - “I reported last year. Nothing happened. Why bother?”
But here’s the reality: if no one reports, the FDA can’t act. If you don’t report, someone else might get hurt next month. Your report could be the one that saves a life.
How to Make Reporting Easier
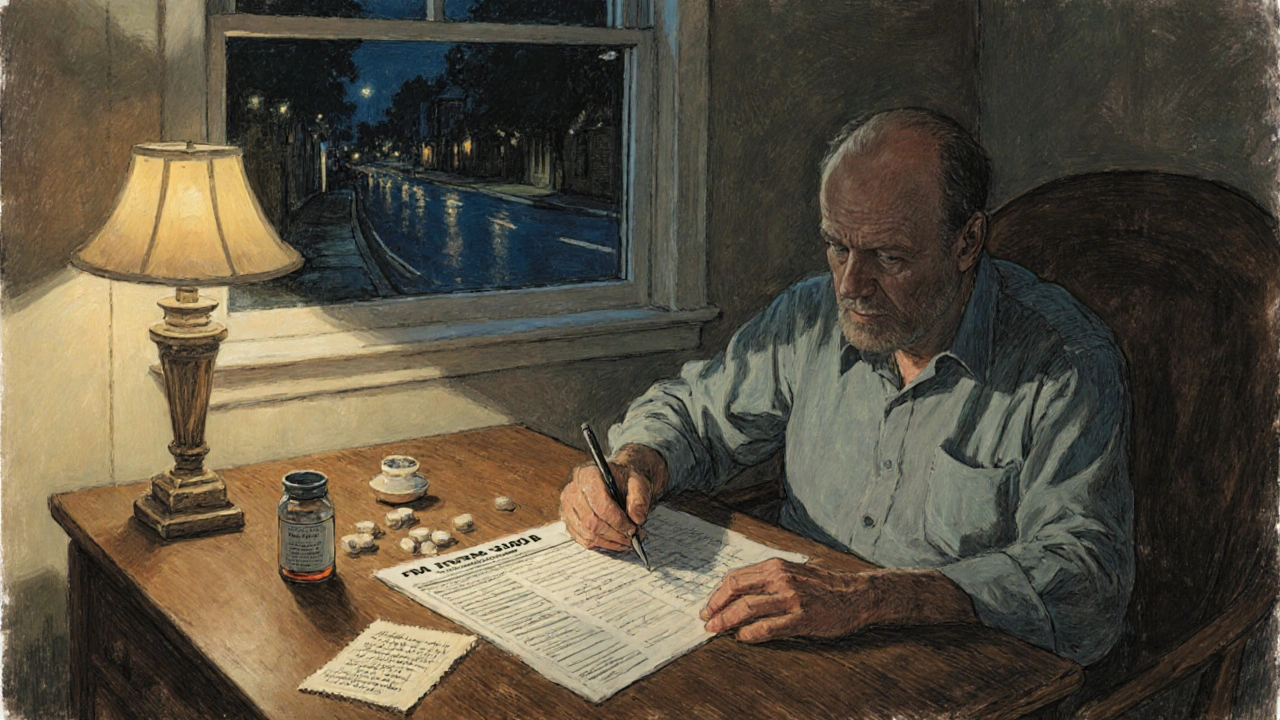
You don’t need to be a medical expert. Here’s how to make it simple:- Keep a quick note - When you notice a side effect, write down: the drug name, when you started it, what happened, and when it started.
- Use the online form - It’s faster than paper. Go to fda.gov/medwatch and click “Report a Problem.”
- Don’t wait for confirmation - If you suspect a link, report it. The FDA doesn’t need proof-they need suspicion.
- Encourage others - If you’re a pharmacist or nurse, help patients fill out Form 3500B. It’s one of the most impactful things you can do.
The FDA is working on improvements. By 2025, they plan to integrate MedWatch reporting directly into electronic health records. That means doctors could click a button during a visit to report a reaction-no extra form needed. But until then, it’s still up to you.
What’s Next for MedWatch?
The FDA’s 2023-2027 plan includes using AI to scan reports faster. Right now, analysts manually review thousands of reports. In the future, software will flag potential patterns before they become crises.They’re also expanding coverage. Since 2019, dietary supplements must be reported more strictly. That’s important-many people assume supplements are “natural” and therefore safe. But they can interact with drugs, cause liver damage, or trigger allergic reactions.
And the volume is growing. In 2022, the FDA approved 37 new drugs-the third-highest year on record. More drugs = more chances for unknown side effects. That means MedWatch is more important than ever.
Final Thought: Your Report Matters
You might think, “I’m just one person. What difference can I make?”Consider this: in 2017, a patient reported a rare but deadly skin reaction linked to a common gout medication. The reaction was so rare, it had never been documented. The FDA reviewed 12 similar reports from across the country. They updated the drug label with a black box warning-the strongest safety alert they have. That warning saved lives.
That patient didn’t know they were helping. They just did what seemed right.
If you’ve had a bad reaction to a medication, you’re not alone. And you’re not powerless. Reporting it through MedWatch is one of the most direct ways to protect others. It takes 15 minutes. It doesn’t cost anything. And it might be the reason someone else avoids a dangerous drug.
Do I need to be a doctor to report an adverse drug reaction to MedWatch?
No. Anyone can report-even patients, family members, or caregivers. The FDA has a special form for consumers called Form 3500B, written in plain language. You don’t need medical training or records. Just describe what happened, when, and what drug you took.
What if I’m not sure the drug caused the reaction?
Report it anyway. The FDA doesn’t require proof of causation. They’re looking for patterns. If 10 people report the same unusual symptom after taking the same drug, that’s a signal. Even if you think it’s a coincidence, your report could be the missing piece.
Can I report a side effect from a supplement or over-the-counter medicine?
Yes. MedWatch covers prescription drugs, over-the-counter medicines, dietary supplements, medical devices, and even some foods and cosmetics. If you had a serious reaction to a vitamin, herbal product, or cold medicine, report it. Supplements aren’t as tightly regulated, so your report helps fill critical safety gaps.
How long does it take to file a MedWatch report?
About 15-20 minutes for patients using the consumer form. Healthcare professionals using the detailed form may take 20-30 minutes. The online version is faster than paper because it includes dropdown menus and auto-fill options. You can save your progress and finish later.
Will I get a response after I report?
Most people don’t. The FDA receives over a million reports a year and can’t respond to each one. But your report is added to a public database used by FDA scientists. If enough similar reports come in, they may investigate further-leading to label changes, warnings, or even drug removals. You won’t hear back, but your report might save someone else’s life.
Is MedWatch the same as the VAERS system?
No. VAERS (Vaccine Adverse Event Reporting System) is only for vaccines. MedWatch covers all FDA-regulated products: drugs, devices, supplements, and cosmetics. If you had a bad reaction to a pill, an IUD, or a dietary supplement, use MedWatch. Only use VAERS for vaccines.
Can I report anonymously?
Yes. You are not required to give your name or contact information. The FDA does not collect personally identifiable information unless you choose to provide it. Your privacy is protected under federal law.

Matthew Peters
November 20, 2025So I took that new blood pressure med last month and woke up with my face looking like a pufferfish. Didn’t think much of it till I saw this post. Filed the MedWatch form yesterday. Took 18 minutes. No doctor note. No stress. Just me, my phone, and a lot of panic. If you’re reading this and had something weird happen? Do it. It’s not about you. It’s about the next person.
Michael Fessler
November 22, 2025As a pharmacist with 14 years in retail, I’ve seen the systemic underreporting firsthand. The 3500B form is intuitive, but most patients don’t even know it exists. We hand them the pamphlet, they nod, and walk out. Meanwhile, the FDA’s FAERS database is drowning in manufacturer reports-85% is absurd. We need mandatory patient education at point-of-sale. Not just for drugs, but for OTCs and supplements too. The lack of causality awareness is a public health blind spot.
daniel lopez
November 23, 2025THIS IS ALL A LIE. The FDA doesn’t care about patients. They’re in bed with Big Pharma. You think they’re gonna pull a drug because some guy in Ohio had a rash? Nah. They wait until 500 people die, then issue a press release that says ‘we’re reviewing.’ Remember Vioxx? They knew for YEARS. MedWatch is a PR stunt. They want you to feel like you’re helping so you stop asking hard questions. The real solution? Ban all drugs. Go herbal. Or better yet-stop trusting the government. #MedWatchScam
Nosipho Mbambo
November 24, 2025...I read this... and... honestly... I'm just... tired. Like, why do I have to do this? I'm not a doctor. I'm not a scientist. I just wanted to take my pill and not die. Why is everything so complicated now? Can't someone just... fix it? I'm not even sure I'm reporting the right thing. I think my knee hurts because of the statin... maybe? I don't know. I'll just... not report. Sorry. 😔
Katie Magnus
November 25, 2025Ugh. Another ‘do your civic duty’ lecture. Like I care if some random person in Nebraska gets a rash from a pill. The FDA has better things to do than babysit every person who thinks their headache is ‘drug-related.’ I’ve had side effects. I didn’t report. I just switched brands. Problem solved. Stop making people feel guilty for not being martyrs.
King Over
November 26, 2025I reported my son’s seizure after the new ADHD med. Took me 20 mins. Got no reply. Still worth it. If it saves one kid it’s done its job. No drama. No fanfare. Just do it.
Johannah Lavin
November 27, 2025Okay I just cried reading this. 🥹 I had a reaction to a supplement last year and I didn’t report it because I thought ‘it’s just vitamins’ and ‘who cares?’ But then I saw someone else’s story online about the same thing and they almost died. I filed my report last week. It felt like I finally did something right. To anyone reading this: your voice matters. Even if it’s quiet. Even if you’re scared. Even if you think you’re overreacting. The FDA needs your signal. 💛
Ravinder Singh
November 27, 2025As someone from India where access to healthcare is uneven, I’ve seen how dangerous unreported reactions can be. In rural clinics, patients are given meds without proper counseling. One woman took a new antibiotic and developed Stevens-Johnson syndrome-she survived, but lost her vision. If someone had reported it earlier, maybe she wouldn’t have been the first. This system? It’s not perfect. But it’s the only shield we’ve got. Share this post. Help a neighbor fill out Form 3500B. A 15-minute act can ripple across continents.
Russ Bergeman
November 29, 2025Wait, so you’re telling me I have to spend 20 minutes reporting every time I get a headache after taking Advil? That’s ridiculous. If it’s not life-threatening, just stop taking it. Why is this even a thing? The FDA is just trying to make people feel useful while doing nothing real. Also, your ‘black box warning’ example? That was a fluke. Most reports go nowhere. Don’t waste your time.
Dana Oralkhan
November 30, 2025I just want to say thank you to the person who wrote this. I’m a nurse and I used to skip reporting because I thought it was pointless. But last month, a patient told me about a weird reaction to her diabetes med. I sat with her and helped her fill out the 3500B form. She cried because no one had ever taken the time before. I realized-I’m not just a nurse. I’m a bridge. And sometimes, the bridge is the only thing keeping someone from falling into the dark.
Jeremy Samuel
December 1, 2025MedWatch? More like MedWaste. I tried to report a reaction to my creatine and the website crashed. Twice. Then I had to sign up for an account. I’m not doing that for a rash. If the FDA can’t make a simple form, maybe they shouldn’t be in charge. Also, I think my weird stomach thing was from the soy sauce. Not the supplement. But whatever. 🤷♂️
Destiny Annamaria
December 3, 2025Y’all are so serious about this. I just took a new vitamin and my skin glowed? Should I report that? 😂 I’m half-joking but also... if you’re gonna make us report every sneeze, can we at least get a cool app? Like ‘MedWatch: The TikTok of Safety’? Add filters. Add memes. Make it fun. I’ll report if I can post a story about it. 🌈💊