21 Dec 2025
- 15 Comments
When you hear Crohn’s disease and ulcerative colitis, they might sound like the same thing-both cause stomach pain, diarrhea, and fatigue. But they’re not. They’re two different diseases under the same umbrella: Inflammatory Bowel Disease (IBD). And understanding the difference isn’t just academic-it changes how you live, what treatments work, and even whether surgery can cure you.
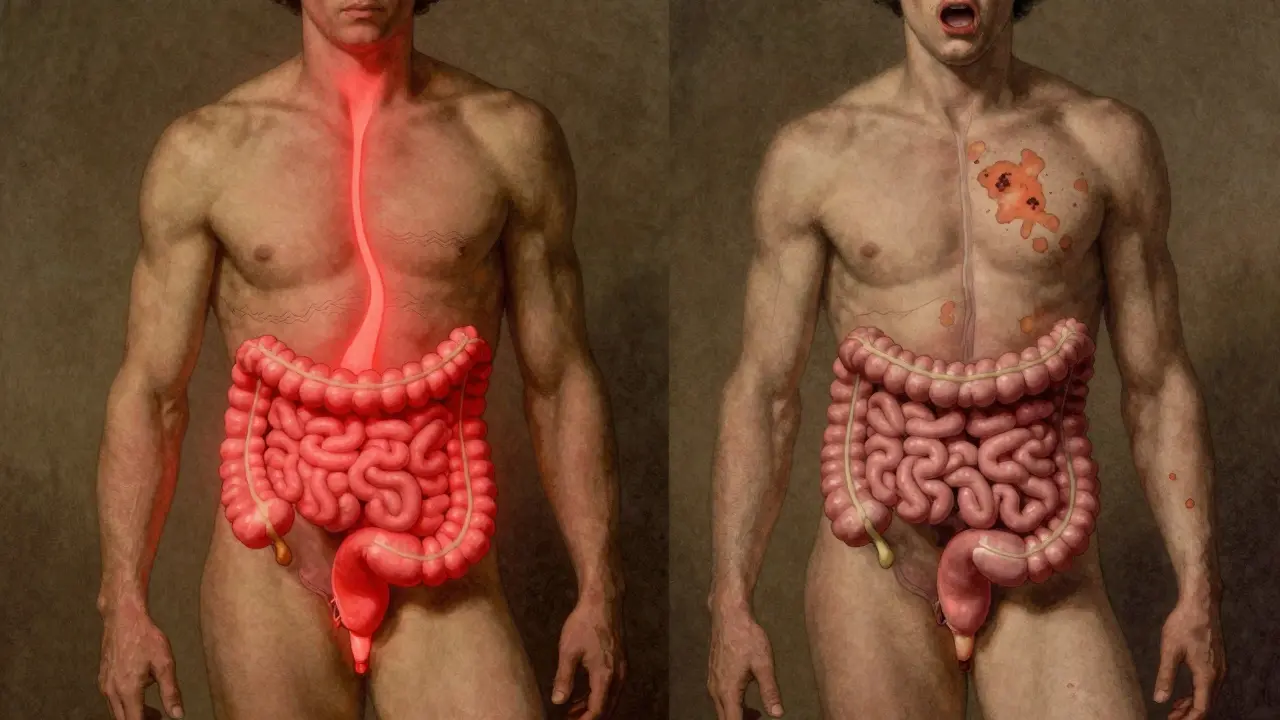
Where It Happens: One Starts at the Rectum, the Other Can Show Up Anywhere
- Ulcerative colitis (UC) only attacks the colon and rectum-the large intestine. It starts at the rectum and moves upward in a continuous line, like a tide flooding a beach. There are no gaps. If you have UC, your entire colon might be inflamed, or just the lower part. But your small intestine? Your stomach? Your esophagus? Those stay untouched.
- Crohn’s disease doesn’t care where it shows up. It can hit your mouth, your esophagus, your stomach, your small intestine, your colon, even your anus. The most common spots? The end of the small intestine (ileum) and the beginning of the colon. But here’s the kicker: it doesn’t go in a straight line. It skips. Healthy patches of tissue sit right next to inflamed ones. Doctors call these "skip lesions." That’s a hallmark of Crohn’s-and it never happens in UC.
How Deep It Goes: Surface vs. Full-Thickness Damage
The lining of your gut has layers. Think of it like an onion. Ulcerative colitis sticks to the top layer-the mucosa. It’s like a sunburn on the inside of your colon. It causes ulcers, bleeding, and mucus, but it doesn’t dig deeper.
Crohn’s disease? It goes all the way through. All layers. The mucosa, the muscle, even the outer covering. That’s called transmural inflammation. And that’s why Crohn’s leads to complications UC rarely does: strictures (narrowing from scar tissue), fistulas (tunnels between organs), and abscesses. These aren’t just uncomfortable-they’re dangerous. About 33% of people with Crohn’s develop strictures over their lifetime. One in four will get a fistula. In UC? Less than 5%.
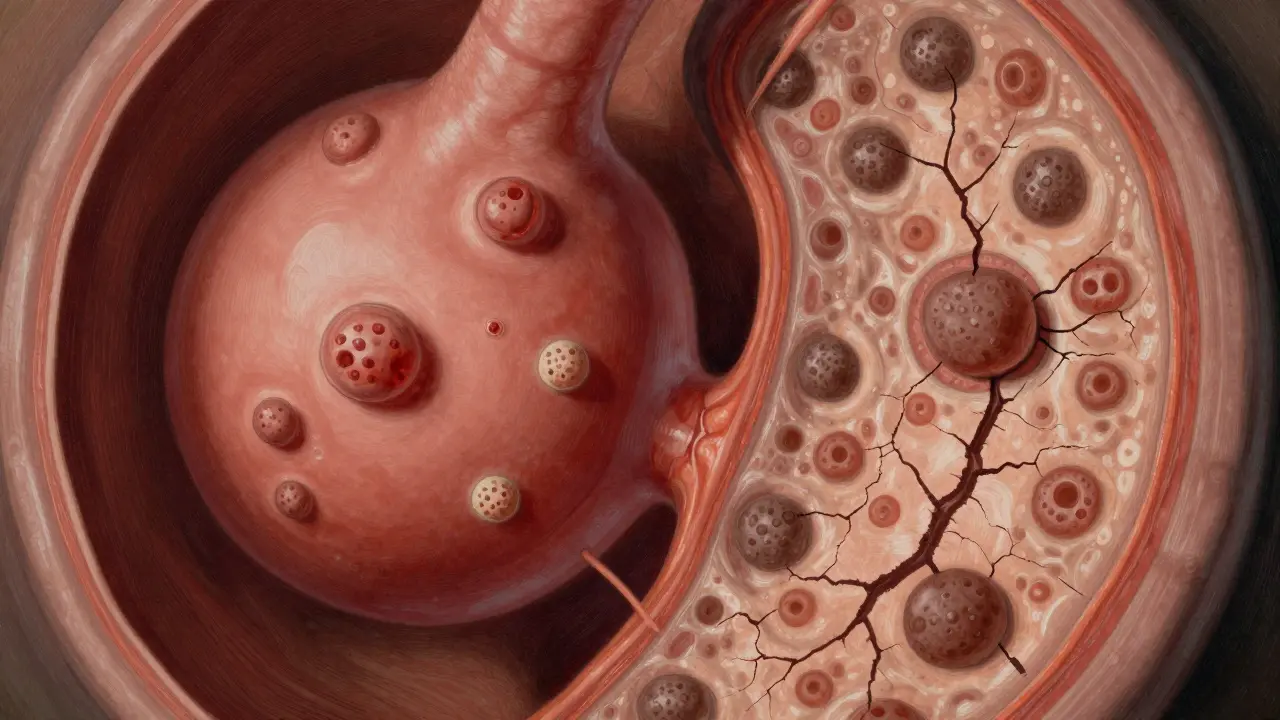
What Shows Up on a Colonoscopy
Doctors use colonoscopy to see inside your gut. In UC, they see a continuous red, raw, bleeding surface. Pseudopolyps-bumps of healing tissue-pop up like islands in a flooded field. That’s textbook UC.
In Crohn’s, it looks different. The lining is swollen, cracked, and covered in little sores that look like cobblestones. There are patches of normal tissue between inflamed areas. Biopsies show granulomas-tiny clumps of immune cells-in about half of Crohn’s cases. Those almost never appear in UC.
But here’s the twist: about 10-15% of cases are unclear at first. Doctors call this "indeterminate colitis." You might start with symptoms that look like UC, but over time, fistulas or small bowel involvement appear-and then it’s reclassified as Crohn’s. That’s why follow-up matters.
Complications: What Could Go Wrong
Both can cause weight loss, fatigue, and anemia. But their big risks are different.
- Ulcerative colitis carries a rare but deadly risk: toxic megacolon. This is when the colon suddenly balloons out, threatening to rupture. It happens in about 5% of severe flares. It’s an emergency. You need surgery fast.
- Crohn’s disease is more likely to cause strictures and fistulas. A fistula can connect your bowel to your bladder, vagina, or skin. Imagine leaking stool into your urine or out through your skin. That’s not rare in Crohn’s-it’s common enough that doctors check for it with MRIs or CT scans.
- Both can cause joint pain, skin rashes, or eye inflammation. But one condition has a unique liver link: primary sclerosing cholangitis (PSC). About 3-7% of UC patients develop this. It’s rare in Crohn’s-under 1%. PSC can lead to liver failure, so UC patients get screened for it.
Testing: Blood, Stool, and Scans
No single test confirms either disease. But some clues help.
- Fecal calprotectin measures gut inflammation. Levels above 250 μg/g are common in active UC (80% of cases) and slightly less so in Crohn’s (65%).
- pANCA antibodies show up in 60-70% of UC patients but only 10-15% of Crohn’s patients. It’s not perfect, but it’s a hint.
- Capsule endoscopy (a pill-sized camera you swallow) finds Crohn’s in the small bowel when colonoscopy looks normal. It catches issues in 70% of suspected cases.
- MRI enterography is the go-to for spotting fistulas and deep inflammation in Crohn’s. It’s not used much for UC.
Treatment: What Works for One Might Not Work for the Other
Both get anti-inflammatories, immunosuppressants, and biologics. But how they’re used differs.
- For UC: Topical treatments work great. Enemas and suppositories with 5-ASAs (like mesalamine) deliver medicine right to the colon. They help 60-80% of mild-to-moderate cases. Oral meds are used too, but the direct delivery makes a big difference.
- For Crohn’s: Since it can affect the whole gut, you need systemic drugs. Pills or injections that work throughout your body. Azathioprine or methotrexate are common starters. Biologics like infliximab or adalimumab help 30-40% of Crohn’s patients reach remission.
- Surprisingly, some biologics work better for one than the other. For example, mirikizumab (a newer drug) is approved for Crohn’s and shows strong results. Etrolizumab is being tested for UC and looks promising.
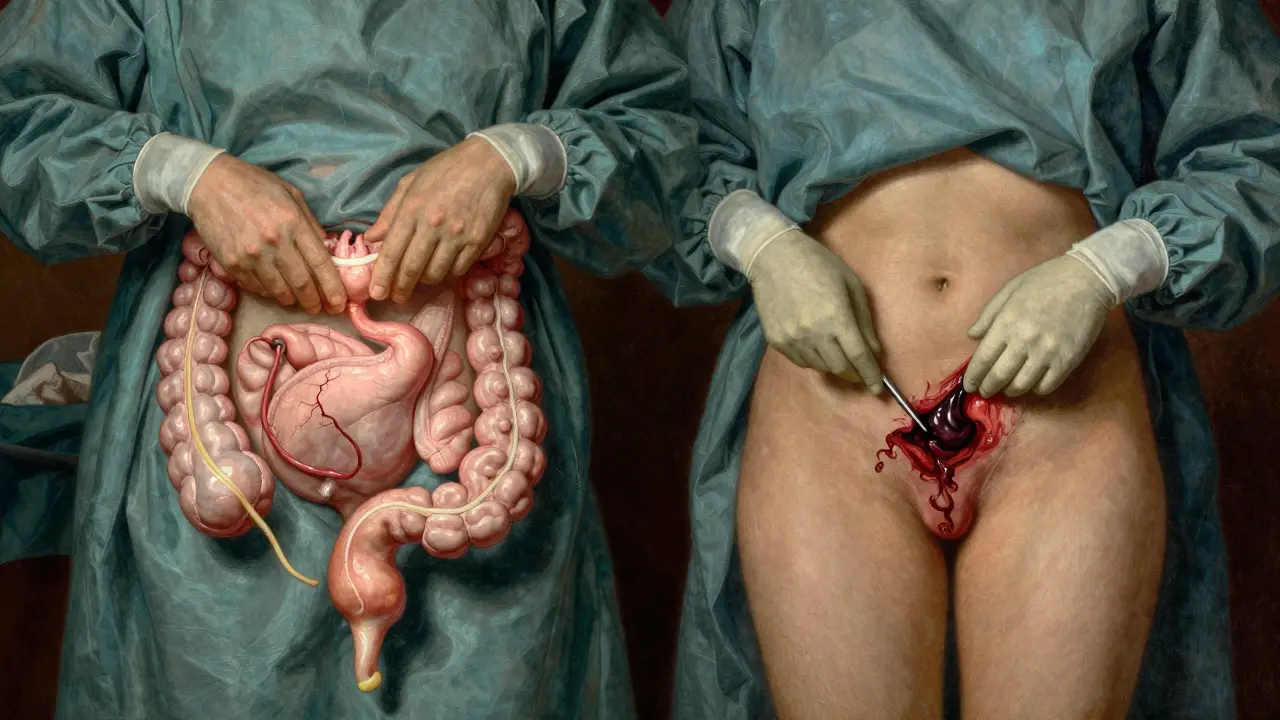
Surgery: Cure vs. Temporary Fix
This is the biggest difference.
- Ulcerative colitis can be cured. Remove the entire colon and rectum, and the disease is gone. The standard surgery is a total proctocolectomy with an ileal pouch (a new internal reservoir made from the small intestine). Most people can poop normally afterward. About 10-15% of UC patients end up with this surgery within 10 years.
- Crohn’s disease cannot be cured with surgery. If you remove a damaged section of bowel, the disease almost always comes back-right next to the surgical site. Half of Crohn’s patients need another surgery within 10 years. Surgery is for complications: blockages, abscesses, or fistulas. It’s not a cure.
What Patients Actually Experience
Real people report real differences.
- UC patients say they feel urgency-like they need to go right now-and rectal bleeding is common (75% report it). Many describe their life as "constantly near a bathroom."
- Crohn’s patients more often talk about nutrition problems. Diarrhea, bloating, weight loss-not just from inflammation, but because their small intestine can’t absorb nutrients. Dairy, fiber, and fatty foods often trigger flares.
- On forums like Reddit’s r/IBD, UC patients blame stress. Crohn’s patients point to food. That’s not just anecdotal-it’s backed by surveys of over 1,200 people.
Cost and Future Hope
IBD is expensive. Severe Crohn’s costs nearly $40,000 a year on average. Severe UC? Around $38,000. Mild cases are cheaper, but still add up.
New treatments are coming. Fecal microbiota transplants (FMT)-transferring healthy gut bacteria-helped 32% of UC patients achieve remission in a 2022 trial. For Crohn’s? Only 22%. That tells us the gut microbiome plays a different role in each disease.
Researchers are now testing drugs that target specific immune pathways. For UC, etrolizumab is in late-stage trials. For Crohn’s, mirikizumab is already approved in some countries. The goal? Not just to control symptoms-but to heal the gut lining and stop the disease before it causes permanent damage.
Bottom Line: It’s Not the Same Disease
Crohn’s disease and ulcerative colitis share symptoms, but they’re not twins. They’re cousins with different DNA. Where they strike, how deep they go, what complications they cause, how they respond to treatment-these differences matter. A misdiagnosis can lead to the wrong treatment, unnecessary surgery, or missed complications.
If you or someone you know has IBD, ask: Is this Crohn’s or UC? And if it’s unclear, ask for follow-up scans, repeat biopsies, and monitoring. Diagnosis isn’t always instant. But getting it right? That’s the key to living well.
Can you have both Crohn’s disease and ulcerative colitis?
No, you cannot have both at the same time. They are two distinct diseases. But about 10-15% of people initially diagnosed with one may later be reclassified as having the other after more symptoms or complications appear. This is called indeterminate colitis. Over time, doctors gather enough evidence-like fistulas or small bowel involvement-to make a clearer call.
Is one worse than the other?
Neither is "worse"-they’re just different. Ulcerative colitis can lead to a life-threatening emergency like toxic megacolon, but it can be cured with surgery. Crohn’s can’t be cured, and it often causes complex complications like fistulas, but it doesn’t usually trigger sudden colon failure. The severity depends on how far it spreads, how deep it goes, and how your body responds to treatment.
Can diet cure IBD?
No diet can cure Crohn’s disease or ulcerative colitis. But diet can help manage symptoms. For example, low-fiber diets often reduce bloating in Crohn’s, while avoiding dairy helps some with lactose intolerance caused by inflammation. UC patients may find that reducing spicy or fried foods cuts down on urgency. Nutrition is support, not a cure.
Do I need to get a colonoscopy every year?
Not every year, but regular colonoscopies are important. If you’ve had ulcerative colitis for 8-10 years, your risk of colon cancer increases. Doctors usually recommend a colonoscopy every 1-2 years after that point. For Crohn’s patients with colon involvement, the same applies. Surveillance helps catch early changes before they turn into cancer.
Can stress cause IBD?
Stress doesn’t cause IBD, but it can trigger flares. The disease is autoimmune-your immune system attacks your gut for reasons still not fully understood. Genetics and gut bacteria play bigger roles. But stress can make inflammation worse. Many UC patients report flares after major life events. Managing stress with therapy, sleep, or mindfulness helps control symptoms.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use, but they do carry risks. They suppress part of your immune system, so you’re more vulnerable to infections like tuberculosis or fungal infections. Before starting, you’ll be screened for TB and hepatitis. Rarely, they’ve been linked to certain cancers, but the risk is low. For most people, the benefits of controlling IBD far outweigh the risks.
Can IBD turn into cancer?
Yes, but it’s not common. Long-standing ulcerative colitis (especially if it affects the whole colon for more than 8-10 years) increases the risk of colon cancer. Crohn’s disease involving the colon also raises the risk, though slightly less. Regular colonoscopies with biopsies help catch precancerous changes early. Controlling inflammation also lowers your cancer risk.

Tony Du bled
December 21, 2025Just had my third flare in 18 months. Took me two years to get diagnosed because everyone thought it was IBS. This post nailed it - Crohn’s isn’t just ‘bad digestion.’ It’s a whole-body war.
Charles Barry
December 22, 2025They’re lying to you. Big Pharma doesn’t want you to know the real cause - glyphosate in your food. UC and Crohn’s? Both caused by Roundup poisoning. The FDA knows. Doctors get paid to ignore it. Your colon isn’t broken - your entire food supply is poisoned.
Rosemary O'Shea
December 23, 2025How quaint. I suppose the only thing more tragic than being diagnosed with IBD is reading about it in a post that uses the phrase ‘tide flooding a beach’ as medical prose. One must wonder if the author believes metaphor substitutes for pathology. The granuloma point was decent, though - at least someone remembered histology.
Jamison Kissh
December 23, 2025If you think about it, the fact that Crohn’s skips around like a broken record while UC just marches in a straight line says something profound about how the immune system loses its way. One’s chaotic, the other’s orderly - maybe that’s why treatments fail so often. We’re treating symptoms, not the underlying chaos of immune miscommunication.
Candy Cotton
December 25, 2025As an American taxpayer, I find it unacceptable that the U.S. healthcare system still treats these diseases like they’re interchangeable. We have the most advanced medical technology on Earth, yet patients are left guessing for years. This is why we need nationalized IBD screening protocols - no more ‘indeterminate colitis’ as a cop-out.
Jeremy Hendriks
December 25, 2025What if the real difference isn’t in the gut but in the soul? Crohn’s is the disease of the wanderer - always searching, never settled. UC is the disease of the rooted - confined, but honest in its confinement. The body reflects the mind. That’s why stress triggers both. We don’t heal tissue. We heal narratives.
Tarun Sharma
December 26, 2025Thank you for this clear breakdown. In India, many still confuse IBD with food poisoning. This will help my patients understand their condition better.
Kiranjit Kaur
December 26, 2025OMG this is so helpful!! 🙌 I’ve had UC for 7 years and finally someone explained why my colonoscopy looked like a ‘flooded field’ - I thought I was the only one who saw it that way 😭 Also, FMT sounds like magic - anyone tried it??
Sai Keerthan Reddy Proddatoori
December 26, 2025They say Crohn’s can’t be cured but they don’t tell you the truth - the government hides the cure. It’s in the Himalayan herbs they banned because it’s too cheap. They want you on biologics for life. Watch the documentary ‘Gut Lies’.
Sam Black
December 27, 2025I’ve been in remission for 5 years with Crohn’s. I didn’t just take meds - I rewrote my entire relationship with food, sleep, and shame. This isn’t just biology. It’s a lifestyle revolution. You don’t fight the disease - you become someone who doesn’t need to.
Johnnie R. Bailey
December 28, 2025One thing missing here: the microbiome’s role in treatment response. FMT works better in UC because the colon’s ecosystem is more intact - it’s a cleaner slate. Crohn’s? The whole gut flora is a warzone. That’s why fecal transplants struggle. We’re not just replacing bugs - we’re rebuilding an entire ecosystem.
Ajay Brahmandam
December 30, 2025My cousin got misdiagnosed as UC for 3 years. Then she developed a fistula. Turns out it was Crohn’s the whole time. Doc said ‘oh well, we’ll just treat it like UC.’ That’s not okay. This post should be required reading for every GI resident.
jenny guachamboza
January 1, 2026wait so if i eat kale and dont cry enough i get crohns?? lol jk but seriously why do they say stress causes flares but not the disease?? like maybe if you just smiled more?? 🤡
Nader Bsyouni
January 1, 2026It’s all about control - the body is a temple but the doctors are priests selling sacraments. Biologics? Just expensive prayers. The real cure is fasting, cold exposure, and silence. But no one wants to hear that because it doesn’t come in a pill bottle with a patent.
Herman Rousseau
January 3, 2026Biggest takeaway for me: UC can be cured with surgery, Crohn’s can’t. That changes everything. If I had to choose? I’d take Crohn’s. At least with UC, you’re one surgery away from losing your identity. With Crohn’s, you still have your colon - even if it’s a battlefield.