15 Dec 2025
- 9 Comments
When a generic drug hits the market, you assume it works just like the brand-name version. But how do we know that for sure? The answer lies in bioequivalence (BE) studies-clinical trials that compare how quickly and completely a drug enters your bloodstream. For decades, these studies were done almost entirely on young, healthy men. That’s changing. Today, regulators are demanding more realistic study populations, especially when it comes to age and sex.
Why Age and Sex Matter in Bioequivalence
Bioequivalence isn’t just about matching pill ingredients. It’s about matching how your body handles them. Men and women don’t process drugs the same way. Age changes how your liver and kidneys work. These differences aren’t minor-they can affect whether a drug works, causes side effects, or even fails entirely in real patients. For example, women often have lower body weight, different fat-to-muscle ratios, and hormonal fluctuations that alter drug absorption. Older adults typically have slower metabolism and reduced kidney function. If a BE study only tests young men, you’re not really testing how the drug performs in the people who actually take it. A 2018 study showed that in small trials (n=12), apparent differences between generic and brand drugs were often just statistical noise caused by a few extreme values. But when the same study was repeated with 36 participants-half male, half female-the differences disappeared. The real issue wasn’t the formulation. It was the flawed study design.FDA Rules: Balance Is Now Required
The U.S. Food and Drug Administration (FDA) updated its guidance in May 2023, and it’s the strictest in the world. If a drug is meant for both men and women, the study must include roughly equal numbers of each. No more 80% male cohorts. No more excuses like “it’s easier to recruit men.” The FDA also requires that studies include adults aged 18 and older. If the drug targets older people-like those with high blood pressure or osteoporosis-you must include participants aged 60 and up. Or, you have to explain why you didn’t. That’s new. Before, sponsors could skip older adults without justification. Now, they can’t. For drugs used almost exclusively by one sex-like hormone therapies or prostate medications-the FDA allows single-sex studies. But you still need to prove why. No guessing. No assumptions. Data-driven decisions only.EMA and ANVISA: Different Approaches, Same Goal
The European Medicines Agency (EMA) takes a more flexible stance. Their 2010 guideline says subjects “could belong to either sex.” That’s it. No requirement for balance. But they do require healthy volunteers aged 18+, with a BMI between 18.5 and 30. No smokers. No pregnant women. No one on chronic meds unless it’s stable and unrelated to the drug being tested. Brazil’s ANVISA is even more specific. They demand a 50:50 split between men and women, and participants must be between 18 and 50 years old. That’s narrower than the FDA’s range. Why? Because ANVISA wants to minimize variability. But this creates its own problem: if a drug is meant for 70-year-olds with kidney disease, excluding them entirely means you’re not testing the real population. The key difference? The FDA wants representation. The EMA wants sensitivity. ANVISA wants control. All three want reliable data. But only the FDA is pushing hard to make sure the people in the study look like the people taking the drug.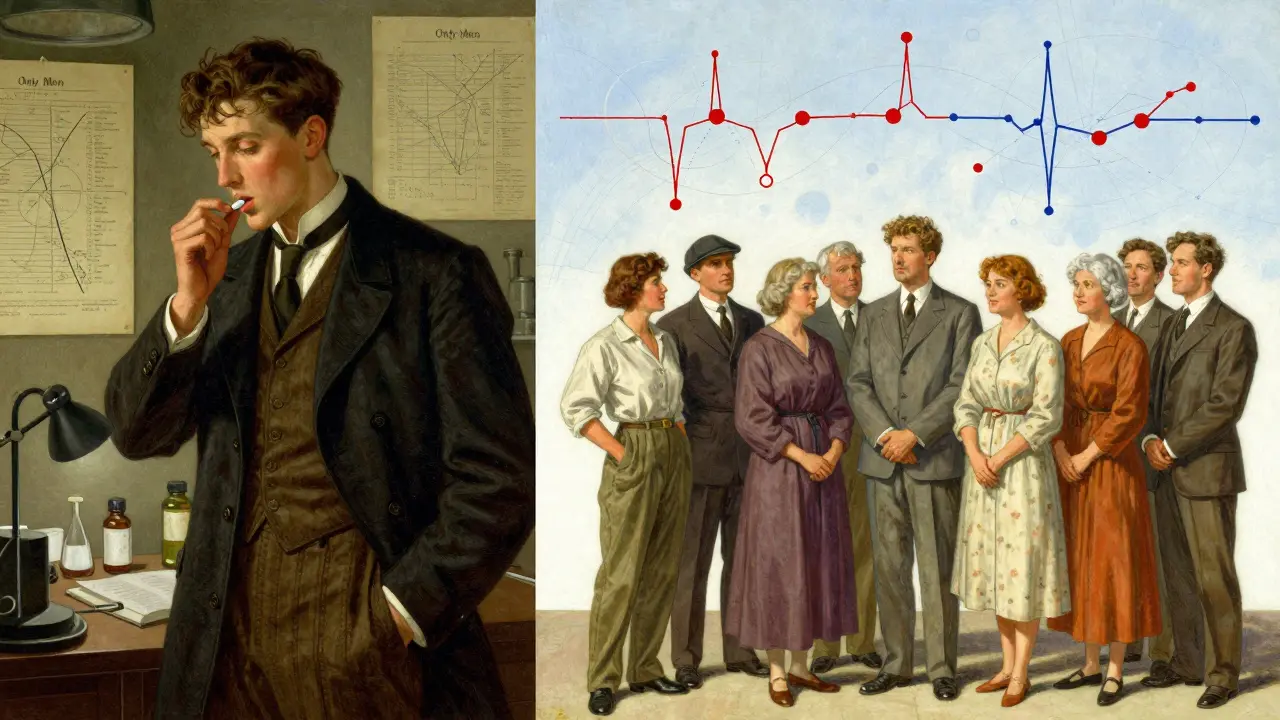
The Real-World Gap: Women Are Still Underrepresented
Even with new rules, reality lags behind policy. Between 2015 and 2020, the FDA reviewed over 1,200 generic drug applications. Only 38% of those studies had between 40% and 60% female participants. The median? Just 32% women. That’s a problem when you consider that 63% of people taking levothyroxine-a common thyroid drug-are women. Yet most BE studies for this drug enrolled fewer than 25% women. How can we say a generic version is safe and effective if we barely tested it on the people who use it most? The reasons are practical, not scientific. Recruiting women for clinical trials takes longer. Sites report a 40% increase in recruitment time for gender-balanced studies. Women are more likely to have caregiving responsibilities, less likely to have flexible work schedules, and more cautious about trial risks. And many sponsors still don’t prioritize it. But pressure is rising. The FDA now requires sponsors to justify any deviation from balanced enrollment. That means more paperwork. More delays. More cost. Some companies are pushing back. Others are adapting. A 2022 survey found that 68% of contract research organizations now run targeted outreach to recruit women-offering childcare, evening appointments, transportation help. But only 29% track sex-specific pharmacokinetic data. That’s still not enough.Statistical Pitfalls and How to Avoid Them
Small studies are dangerous in bioequivalence. If you enroll only 12 people, and one woman has an unusually high absorption rate, that one outlier can make the whole study look like the drugs aren’t equivalent. That’s not science-it’s luck. The fix? Larger samples. At least 24 participants, ideally 36. And stratified randomization-making sure men and women are evenly split across the two drug groups. That way, if one group has a few outliers, they’re balanced out. Also, pre-specify your analysis. Don’t just look at the whole group. Look at men and women separately. If the generic drug performs differently in women than in men, you need to know. The FDA now expects this. The EMA doesn’t require it-but if you don’t do it, and later a woman has a bad reaction, you’ll be asked why you didn’t check.
What’s Next? The Future of Inclusive Bioequivalence
The next wave of change is coming. Researchers at the University of Toronto found that 37% of commonly tested drugs are cleared from the body 15-22% faster in men than in women. That’s not a small difference. For drugs with a narrow therapeutic index-like warfarin or digoxin-this could mean the difference between a safe dose and a toxic one. The National Academies of Sciences recommended in 2021 that regulators develop sex-specific bioequivalence criteria for these high-risk drugs. The FDA’s 2023-2027 strategic plan lists “enhancing representation of diverse populations” as a top priority. The EMA is reviewing its 2010 guideline and may update it in 2024. We’re moving toward a future where bioequivalence isn’t just about matching a pill. It’s about matching a person. Age, sex, weight, metabolism-all these factors matter. The science is clear. The regulations are catching up. The question now is: will industry keep dragging its feet, or will it finally design studies that reflect the real world?What Sponsors Should Do Today
If you’re developing a generic drug, here’s what you need to do right now:- Design your BE study to reflect the target population. If it’s for older adults, include them.
- If the drug is used by both men and women, enroll a 50:50 split. Don’t wait for the FDA to ask.
- Use stratified randomization. Track sex-specific PK data. Pre-specify subgroup analysis.
- Document your choices. If you exclude a group, justify it with data-not convenience.
- Start recruiting early. Women need more time. Offer flexibility.


jeremy carroll
December 15, 2025finally someone says it! i've been in pharma for 12 years and we still do these 12-man studies like it's 1995. my boss even said 'women are harder to recruit' like that's an excuse and not a failure of planning. 🤦♂️
Edward Stevens
December 17, 2025oh wow, the FDA actually cares about women now? who knew. next they'll ask if the drug works for people who aren't 25-year-old college guys who lift weights and drink protein shakes. 🙃
Alexis Wright
December 17, 2025This is not progress. This is performative regulation. You think including 50% women in a BE study magically fixes systemic pharmacokinetic bias? No. You need sex-specific bioequivalence thresholds, not token enrollment. The FDA’s 2023 guidance is a band-aid on a hemorrhage. The data shows women clear 15-22% faster for 37% of drugs. You’re not testing bioequivalence-you’re testing whether your statistical model can survive an outlier. And you’re still not measuring metabolites. You’re not even close.
Tim Bartik
December 17, 2025bruh why are we even doing this? if a drug works for a 22yo guy, it works for everyone. women are just more sensitive and old people are just broken. stop overcomplicating it. if your grandma gets sick on the generic, maybe she shouldn't be takin' it. #americanpride
Sinéad Griffin
December 19, 2025i’m a 47yo woman on levothyroxine and i’ve had 3 different generics in 5 years. 2 made me jittery, 1 made me feel like a zombie. none of the BE studies i’ve read even mentioned my age or sex. how is this legal? 😤
Wade Mercer
December 19, 2025The fact that we still need to argue this points to a deeper moral failure in clinical research. We are not just testing drugs-we are testing human dignity. Every time we exclude a demographic, we are saying their health doesn't matter as much. That’s not science. That’s negligence dressed in white coats.
Sarthak Jain
December 20, 2025in india we have same prob but worse. many generic studies use only 10-12 healthy young males. i once saw a study for a diabetes drug where all participants were 20-25yo men. the drug was for 60+ diabetics. how? 🤔 i think regulators need to mandate subgroup analysis. also, maybe use real-world data? like ehr? just a thought.
Daniel Thompson
December 21, 2025I'm not opposed to diversity in trials, but the regulatory burden is becoming absurd. We're spending 40% more on recruitment, delaying launches by 8-12 months, and still getting no additional clinical benefit from stratified analysis in 80% of cases. The FDA's approach is noble, but it's creating a compliance theater that hurts patients by delaying access to affordable meds.
Daniel Wevik
December 22, 2025This is the future. We’re moving from 'one-size-fits-all' to 'right-dose-for-the-right-body.' It’s not just ethical-it’s pharmacologically necessary. Companies that resist this are betting on outdated science. The data is clear: sex and age aren’t variables to control for-they’re key parameters. Start designing for real people, not lab rats.