9 Dec 2025
- 15 Comments
Many people assume that if they have long-term care insurance, it will pay for everything when they move into a nursing home - including their daily medications. That’s not true. Long-term care insurance doesn’t cover prescription drugs, not even generic ones. It pays for room and board, help with bathing, dressing, and eating - the daily support you need when you can’t live independently. But your pills? Those come from somewhere else.
Why Long-Term Care Insurance Doesn’t Cover Medications
Long-term care insurance was never designed to pay for medical treatments. It’s meant to cover custodial care - the kind of help that keeps you safe and clean, not the kind that fixes your illness. If you need insulin, blood pressure pills, or antibiotics, those are considered medical expenses. And medical expenses? They fall under health insurance, not long-term care coverage. This isn’t a loophole. It’s by design. Since the 1970s, when modern long-term care policies first appeared, insurers have kept medical care and custodial care separate. That changed in 2006 with Medicare Part D, which created a clear path for drug coverage in nursing homes. But long-term care insurance never got an update to include prescriptions. Even today, if you’re in a nursing home and your policy says it covers "all care," read the fine print. It’ll say something like "room, board, and personal assistance" - not "medications."Who Actually Pays for Your Generic Drugs in a Nursing Home?
If not long-term care insurance, then who? For most people in nursing homes, the answer is Medicare Part D. About 82% of prescription drugs in U.S. nursing homes are paid for by Part D plans. That’s not a small number - it’s the backbone of drug coverage in this setting. Generic drugs make up about 90% of all prescriptions given in nursing homes. They’re cheaper, just as effective, and Part D plans love them. Why? Because they cost less. Most Part D plans charge a lower copay for generics - often $1 to $5 per prescription - compared to $10 or more for brand-name drugs. That’s good news for residents, but only if they’re enrolled. For people with low income, Medicaid steps in. If you’re dually eligible - meaning you get both Medicare and Medicaid - Medicaid covers your drugs if you’re not in a Medicare-covered stay. For veterans, the Veterans Administration handles it, but that’s only 0.2% of cases. The scary part? Around 9% of nursing home residents - nearly 30,000 people - have no drug coverage at all. They pay out of pocket, or get help from charity programs that run out. That’s not a glitch. It’s a system failure.How Medicare Part D Works in Nursing Homes
Part D doesn’t just hand out pills. It works through a complex web of rules. Each plan has a formulary - a list of approved drugs. Not every generic is covered on every plan. Some plans limit which brands of a drug they’ll pay for. Others require prior authorization before you can get a certain pill. Nursing homes have to figure out which plan each resident is on. Then they have to check if their pharmacy works with that plan. Then they have to see if the resident’s meds are on the formulary. If not, they file an exception request. That process can take days. During that time, the resident might go without their medication. One study found that facilities spend 10 to 15 hours a week just managing drug coverage issues. That’s over $28,000 a year in staff time. And that’s not counting the stress on families trying to understand why their parent’s blood pressure pill was suddenly denied.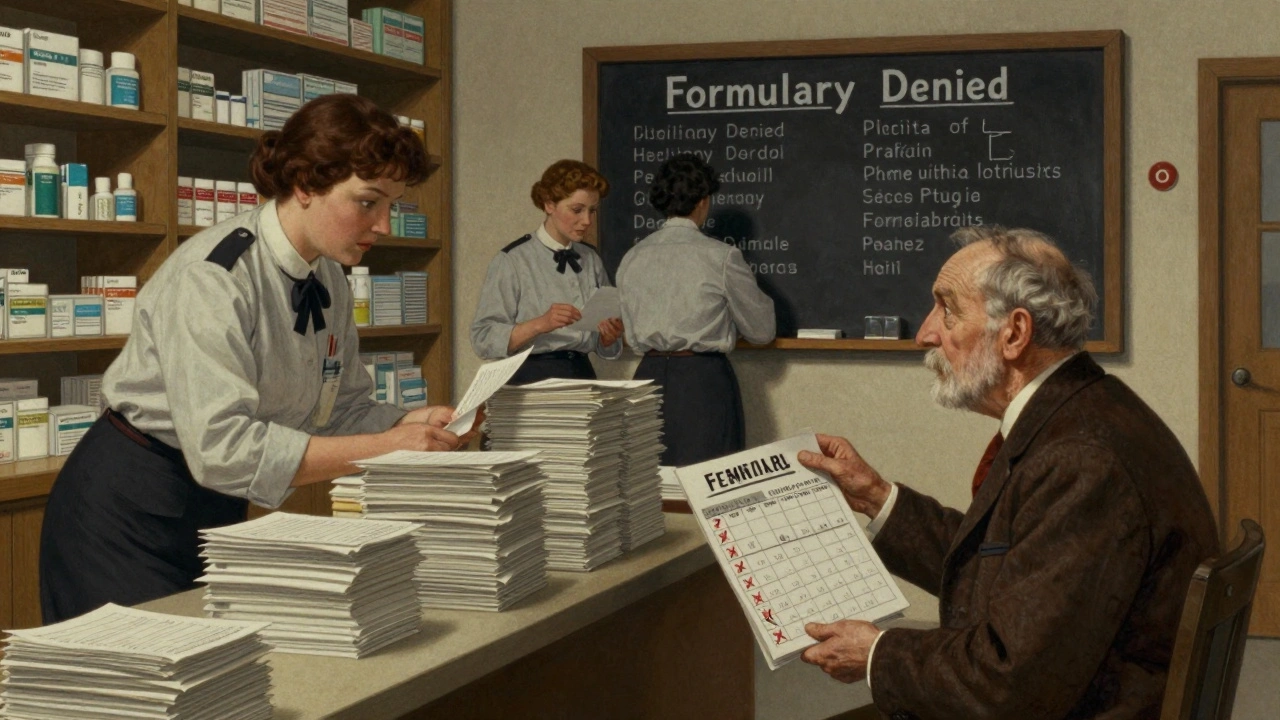
The Formulary Problem
Just because a drug is generic doesn’t mean it’s automatically covered. Part D plans can still block it if it’s not on their list. And they often do - especially if a cheaper alternative exists. For example, if a resident takes a generic version of a blood thinner, but the plan only covers a different generic brand, the facility has to request an exception. The resident might get a new prescription, or worse - go without for days while the paperwork moves. Medicare requires plans to cover all drugs on the national Part D formulary, but they can still restrict access. And they’re not required to approve exceptions quickly. For nursing home residents, delays can mean hospital visits - and higher costs for everyone. The good news? Starting in 2025, the Inflation Reduction Act will cap out-of-pocket drug costs at $2,000 a year. That’s a big win. But it doesn’t fix the formulary mess. It just limits how much you pay if you get stuck with an expensive drug.What Happens When You Don’t Have Coverage?
If you’re one of the 9% without drug coverage, you’re on your own. Some families pay out of pocket. Others rely on state assistance programs, which vary wildly by location. A few get help from pharmaceutical companies’ patient assistance programs - but those often require paperwork, income proof, and waiting lists. One 2020 study showed that residents without Part D got far fewer prescriptions than those who had it. Not because they didn’t need the drugs - because they couldn’t afford them. That’s not just inconvenient. It’s dangerous. Missed doses of heart meds, diabetes pills, or antibiotics can lead to hospitalization, infections, or even death.
What Should You Do Before Moving Into a Nursing Home?
If you or a loved one is considering long-term care:- Check if you’re enrolled in Medicare Part D. If not, sign up immediately. Late enrollment penalties can add up.
- Ask the nursing home which pharmacies they work with. Not all pharmacies accept all Part D plans.
- Get a copy of your current drug list. Bring it with you.
- Ask the facility’s social worker or pharmacy liaison: "Which Part D plans do you accept? What’s the process if a drug isn’t covered?" Write it down.
- Don’t assume long-term care insurance covers meds. It doesn’t. Plan for it separately.


Larry Lieberman
December 10, 2025So let me get this straight - my grandma’s $5 insulin is covered by Medicare Part D, but the $200/month pill for her arthritis? Nope, not unless it’s on some random formulary list 🤦♂️. And we’re supposed to be grateful for the $2k cap in 2025? Bro, that’s just damage control after years of neglect. 😔💊
Lisa Whitesel
December 10, 2025Long-term care insurance never covered meds. That’s not a flaw. That’s the design. If you think it should, you didn’t read the policy. End of story.
Richard Eite
December 12, 2025Americans are so lazy they think insurance should cover everything. Get a job. Pay cash. Stop relying on government handouts. This is why our system is broken.
iswarya bala
December 13, 2025omg this is so true!! i had to help my auntie in delhi and she had to pay outta pocket for her meds for 3 months 😭 no one told her about part d. pls share this more!!
Philippa Barraclough
December 13, 2025The structural separation between custodial and medical care is a relic of 20th-century healthcare financing. The fact that we still rely on a patchwork of Part D, Medicaid, and charity programs for essential medications in nursing homes reveals a fundamental failure in policy integration. The administrative burden on staff - 10 to 15 hours weekly - is not merely inefficient; it is ethically indefensible when human health is at stake.
Delaine Kiara
December 13, 2025They say ‘formularies vary by state’ like it’s some cute little quirk. It’s not. It’s a death sentence for people who can’t navigate bureaucracy. I’ve seen it. My uncle went without his anticoagulant for 11 days because his plan switched pharmacies and no one told the nursing home. He ended up in the ER with a stroke. This isn’t a system. It’s a minefield.
Katherine Chan
December 14, 2025Thank you for writing this. So many families are flying blind. Please share this with your local Area Agency on Aging. Knowledge is power - and maybe, just maybe, it can save a life. 💪❤️
Tim Tinh
December 15, 2025Man I wish my cousin who works in a nursing home in Texas knew this. She’s been stressing over meds for months. I’m forwarding this to her right now. Also - generic doesn’t mean ‘cheap junk’. It means ‘same drug, less markup’. Gotta educate folks.
Rich Paul
December 17, 2025Formulary tiering, prior authorization, step therapy - these are cost-containment mechanisms, not failures. The system is working exactly as intended: prioritize low-cost generics, incentivize utilization management, and externalize administrative burden to facilities. If you can’t handle the complexity, don’t get old.
Katherine Rodgers
December 18, 2025Wow. So the government lets old people die because they forgot to sign up for Part D? Shocking. Next they’ll say ‘you should’ve bought life insurance’ before you got hit by a bus. 😂
Lauren Dare
December 18, 2025The 9% without coverage? That’s not a ‘system failure’. That’s a market signal. If you can’t afford to plan ahead, you shouldn’t be in a nursing home. The system isn’t broken - it’s filtering out the unprepared.
Gilbert Lacasandile
December 20, 2025I think this is really important. Maybe we need a national standard for formularies in nursing homes? Like, if you’re in a facility, your meds should be covered if they’re on the national list. No more 50 different rules for 50 states. Just a thought.
Courtney Black
December 20, 2025Medicare Part D is the silent guardian of the elderly. It’s not glamorous. No one talks about it. But without it, nursing homes would be death rows. And yet we treat it like an afterthought - like a bonus feature, not the foundation. We build monuments to soldiers and astronauts, but we let the people who kept us alive as children go without their pills because the paperwork was too complicated. That’s not negligence. That’s a moral collapse.
It’s not about policy. It’s about dignity. A person who can’t swallow their own pills shouldn’t have to beg for them. A grandmother who needs insulin shouldn’t be told, ‘We’ll get back to you in 72 hours.’ That’s not healthcare. That’s bureaucracy with a stethoscope.
And yes, long-term care insurance doesn’t cover meds. But why? Because in 1973, someone decided that care and medicine were separate. That was wrong then. It’s criminal now. We don’t separate food from eating. We don’t separate oxygen from breathing. Why do we separate pills from survival?
And the $2,000 cap in 2025? That’s a bandage on a hemorrhage. It helps the person who gets the expensive drug. But what about the 30,000 who get nothing? Who pays for them? The state? The family? The church? The pharmacy? No one. That’s the real failure. Not the formulary. Not the delay. The silence.
We are the generation that watched our parents die in hospital beds while we scrolled through memes about ‘healthcare reform.’ We knew. We read the reports. We saw the headlines. And we did nothing. So don’t tell me the system is broken. Tell me why we let it be.
Ruth Witte
December 20, 2025THIS! My mom’s pharmacy changed her blood pressure med last month and she went 4 days without it 😭 I almost lost it. If you’re reading this - PLEASE talk to your family about meds BEFORE they move in. It’s the most important thing!
And yes, generics are the heroes here. 💪💊 #PartDIsLife
Simran Chettiar
December 21, 2025It is an undeniable truth that the contemporary American healthcare architecture, particularly as it pertains to the elderly population residing in institutionalized settings, exhibits profound systemic dissonance. The bifurcation between custodial and pharmaceutical care is not merely an administrative artifact; it is a philosophical indictment of our societal values. To treat the human body as a collection of discrete, compartmentalized functions - nutrition, mobility, cognition, pharmacology - is to misunderstand the very essence of care. Medication is not an add-on. It is the continuation of life itself. To delay a pill because of formulary constraints is to delay the possibility of continued existence. The fact that nursing homes spend 10 to 15 hours weekly on bureaucratic mediation rather than therapeutic intervention is not inefficiency - it is dehumanization.
Furthermore, the regional variance in formulary coverage is not merely inconvenient; it is a violation of equity. A resident in Ohio deserves the same access to a generic antihypertensive as a resident in California. The notion that healthcare access should be determined by zip code is an affront to the principle of universal human dignity. The 2025 cap on out-of-pocket expenses, while commendable, is a palliative measure. It does not address the root cause: the absence of a unified, nationally standardized pharmaceutical coverage framework for long-term care residents.
It is time we recognize that the right to medication is not a privilege granted by insurance contracts, but a fundamental human right. Until that recognition is codified into law, we are not a society that cares for its elderly - we are a society that merely tolerates them.