20 Nov 2025
- 11 Comments
Every year, Americans spend over $370 billion on prescription drugs. A huge chunk of that - nearly 90% of all prescriptions filled - goes to generic medications. And yet, many people still hesitate to switch from brand-name drugs, worried that cheaper means worse. What if you could cut your monthly drug bill by 80% without risking your health? The truth is, you can - if you know how to do it right.
Generics Are Not Second-Class Drugs
Generic drugs contain the exact same active ingredients as their brand-name counterparts. That means if you’re taking lisinopril for high blood pressure, the generic version has the same molecule, the same strength, and the same way of working in your body as Zestril or Prinivil. The FDA doesn’t approve generics unless they match the brand in dosage, effectiveness, safety, and how quickly they’re absorbed. In fact, the same companies that make brand-name drugs often make the generic versions too - just under a different label.How Much Can You Really Save?
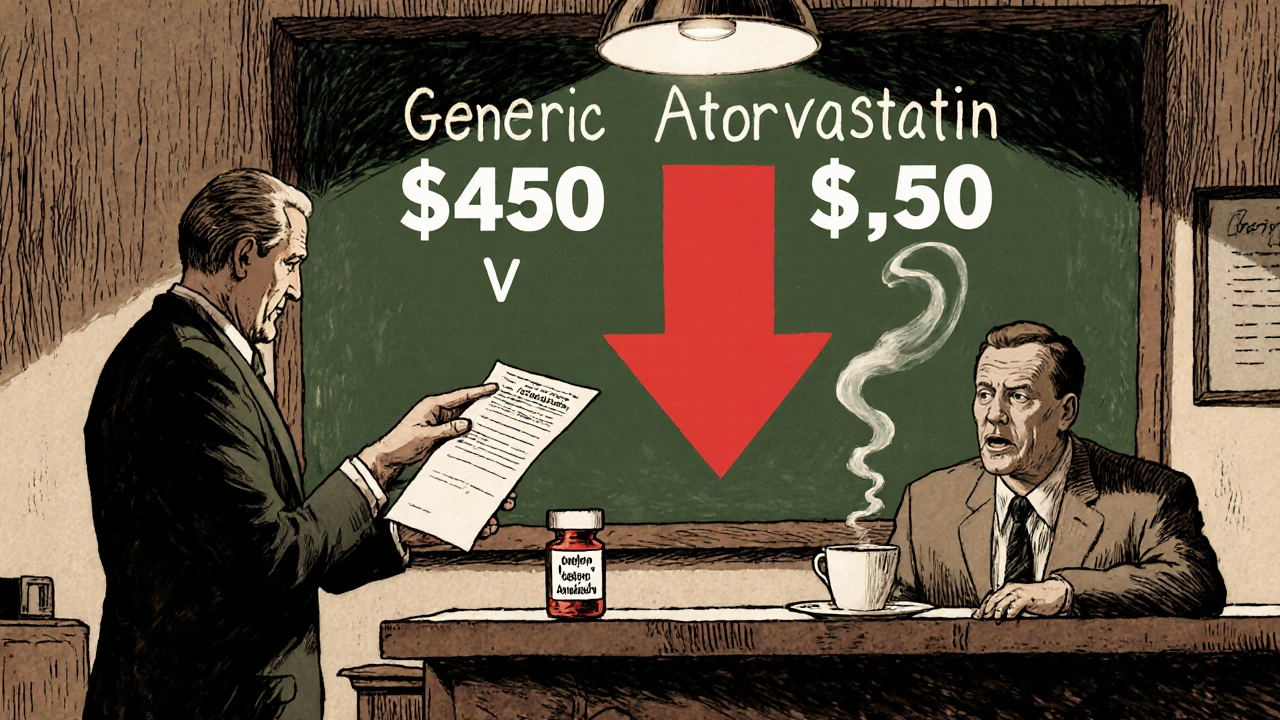
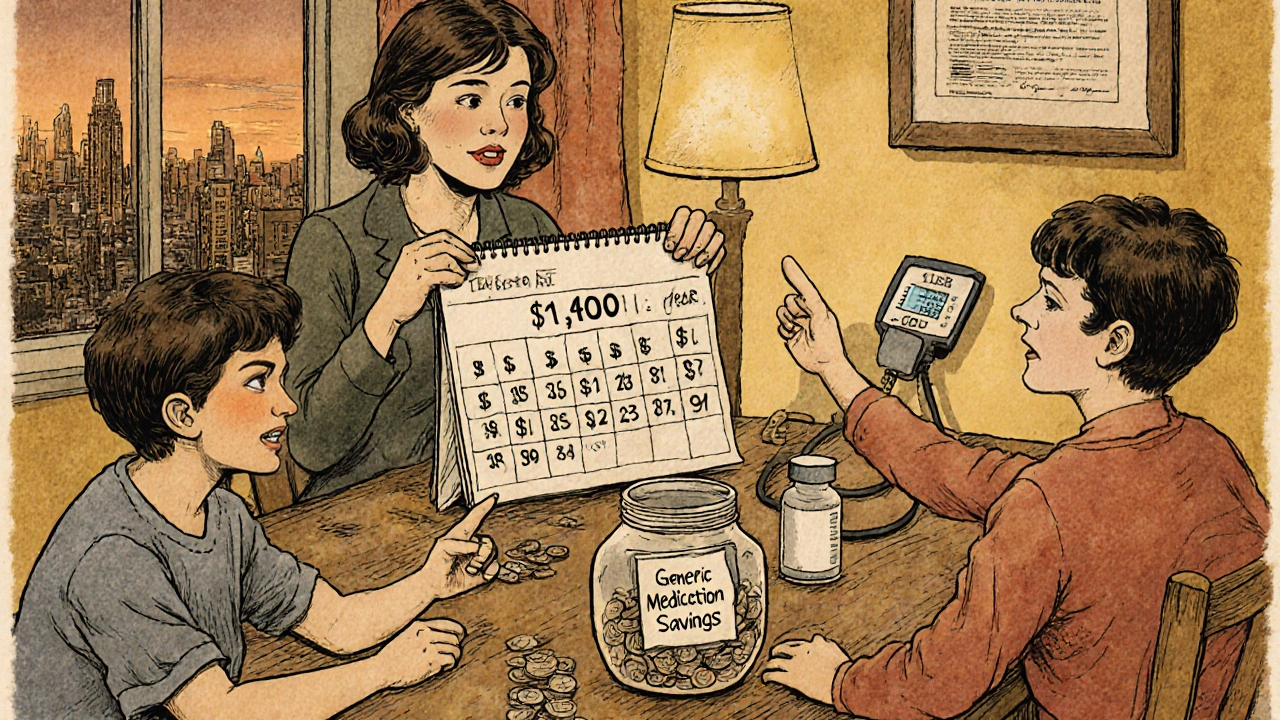
The cost difference isn’t just noticeable - it’s dramatic. A 30-day supply of brand-name Lipitor (atorvastatin) can cost over $450. The generic? As low as $0.50 at major pharmacies like Walmart or Costco. Plavix (clopidogrel) runs around $380 per month. Generic clopidogrel? About $1.20. For people on multiple medications, switching to generics can mean saving $500 to $2,000 a year. That’s not pocket change - that’s rent, groceries, or a car payment.When Generics Are Just as Safe - and Sometimes Safer
A 2020 study in Nature Communications looked at 17 cardiovascular drugs and found that in 10 of them, patients taking generics had fewer deaths. In 11, they had fewer major heart problems. Another study tracked 2.3 million people and found no increased risk of heart attacks or strokes with generic statins - as long as patients stayed on the same manufacturer. That’s the key: consistency. For most drugs - blood pressure meds, antidepressants, antibiotics, diabetes pills - generics are just as safe and effective. The FDA has reviewed over 12,000 generic applications since 2022. Not a single one was approved without proving it works the same way as the brand.The Exceptions: When You Need to Be Careful
Not all drugs are created equal when it comes to switching. Some have what’s called a narrow therapeutic index - meaning the difference between a dose that works and one that’s dangerous is very small. These include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (anti-seizure)
- Sirolimus and cyclosporine (immunosuppressants)
What’s Really in a Generic Pill?
The only differences between a generic and brand-name drug are in the inactive ingredients - the fillers, dyes, and coatings. These don’t affect how the drug works. But they can affect how the pill looks. Your generic might be white instead of blue. It might be round instead of oval. It might say “Watson” or “Teva” instead of “Pfizer.” That’s normal. But if your pill suddenly changes color, shape, or imprint - and you haven’t asked for it - that’s a red flag. A 2021 study found that 65% of adverse events linked to generics came from unexpected manufacturer switches, not poor quality. Always check the label. If it’s different, ask your pharmacist: “Is this the same manufacturer as before?”How to Switch Safely
You don’t have to guess. Here’s a simple, three-step plan:- Ask your pharmacist: “Is this generic from an FDA-inspected facility?” You can check this yourself using the FDA’s Drugs@FDA database. All legal generics are made in inspected plants - same as brand-name drugs.
- Check if multiple generics exist: If there are three or four brands of the same generic, that means competition is driving prices down. That’s good for you.
- Ask about narrow therapeutic index drugs: If you’re on warfarin, levothyroxine, or an anti-seizure med, say: “Can I stay on the same manufacturer?”
What to Do If You Feel Different
Some people report feeling off after switching - fatigue, dizziness, mood changes, or worsening symptoms. That doesn’t mean the drug is bad. It might mean your body adjusted to a different filler, or you switched manufacturers without realizing it. If you notice a change:- Don’t stop taking it.
- Write down what changed and when.
- Call your doctor or pharmacist. Say: “I switched to the generic and I’m feeling [symptom]. Can we check my levels?”
Why Some Doctors Still Hesitate
You might hear your doctor say, “I prefer the brand.” That’s often not about safety - it’s about habit. Many were trained in an era when generics had a reputation for inconsistency. But that was decades ago. Today’s generics are held to the same standards as brand-name drugs - same manufacturing rules, same testing, same inspections. A 2019 Harvard Health report quoted Dr. Niteesh Choudhry: “There is really no hard proof at this point that generic medications are any less effective or safe than the originals.” The American Heart Association agrees: generics are safe for most heart conditions - just be cautious with narrow therapeutic index drugs.How Generics Help Everyone - Even If You Don’t Use Them
When you choose a generic, you’re not just saving money for yourself. You’re helping lower the overall cost of healthcare. Insurance companies pay less. Medicare spends less. Tax dollars go further. That means more people can afford care. It means drug companies have less leverage to raise prices on brand-name drugs. It means the system works better for everyone. In 2023, generics saved the U.S. healthcare system $1.97 trillion since 2009. That’s not a number - that’s millions of people who got the medicine they needed because it was affordable.What’s Next? Biosimilars and Better Oversight
The future of generics is getting even better. Biosimilars - generics for complex biologic drugs like Humira or Enbrel - are now approved for cancer, arthritis, and autoimmune diseases. The FDA expects them to save $300 billion by 2030. The agency is also cracking down on shortages. In 2024, it launched a Generic Drug Shortage Task Force after amoxicillin and Adderall ran out. New rules require manufacturers to use modern production methods by 2026, making supply chains more reliable.You Don’t Have to Choose Between Cost and Care
You can save hundreds - even thousands - of dollars a year on prescriptions without risking your health. Generics are not a compromise. They’re the standard. For most people, they’re just as safe, just as effective, and infinitely more affordable. The trick is knowing when to ask questions. When to stick with the same manufacturer. When to test your levels. When to speak up. Your health isn’t about the brand on the bottle. It’s about the medicine inside. And that’s exactly the same.Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of medications, generics are just as effective. The FDA requires them to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence - meaning they work the same way in your body. Studies involving millions of patients show no difference in outcomes for drugs like blood pressure meds, statins, antibiotics, and antidepressants.
Can switching to a generic cause side effects?
Side effects from the active ingredient are the same. But sometimes, the inactive ingredients (like dyes or fillers) can cause minor reactions in sensitive people - like stomach upset or rash. These are rare and usually go away within a week or two. If you notice new symptoms after switching, talk to your pharmacist or doctor. It could also mean you switched manufacturers - which can sometimes affect how the drug is absorbed, especially for narrow therapeutic index drugs.
Which drugs should I avoid switching to generic?
Avoid switching generics for drugs with a narrow therapeutic index - where small changes in blood levels can be dangerous. These include warfarin (Coumadin), levothyroxine (Synthroid), phenytoin (Dilantin), and some anti-seizure or transplant drugs. For these, stick with the same manufacturer. Ask your doctor if you’re unsure. Never switch these without medical guidance.
Why do generic pills look different?
By law, generic pills can’t look identical to brand-name pills - that would be trademark infringement. So they use different colors, shapes, or imprints. This doesn’t affect how the drug works. But if your pill suddenly changes appearance and you didn’t ask for it, check the label. It might be a different manufacturer. Always verify the name on the bottle and ask your pharmacist if you’re unsure.
Can I trust generics made overseas?
Yes. The FDA inspects all manufacturing facilities - whether in the U.S., India, China, or elsewhere - using the same strict standards. Over 50% of generic drugs sold in the U.S. are made overseas, but every facility must pass FDA inspections. You can verify this by checking the FDA’s Drugs@FDA database. If a generic is legally sold in the U.S., it’s been approved and inspected.
Will my insurance cover generics?
Almost always - and at a much lower cost. Most insurance plans require you to try the generic first. If you insist on the brand, you’ll pay more - sometimes 10x more. Many pharmacies offer generics for $4 or less with no insurance. Always ask your pharmacist: “What’s the cash price for the generic?” It’s often cheaper than your co-pay.
Do generics take longer to work?
No. Generics must prove they’re absorbed into your bloodstream at the same rate and to the same extent as the brand-name drug. The FDA requires bioequivalence testing in healthy volunteers. For most drugs, absorption happens within minutes of each other. If you feel a delay, it’s likely psychological - or you switched manufacturers. Don’t assume it’s the generic’s fault.
What if I’m on a long-term medication? Should I stay on the brand?
For most long-term meds - like metformin, atorvastatin, or sertraline - generics are not only safe, they’re the smarter choice. Staying on brand costs hundreds more per month. The only reason to stay on brand is if you’ve had a bad reaction to a specific generic - and even then, try another manufacturer before giving up. Many people switch back and forth between generics without issue. The key is consistency: once you find one that works, stick with it.

David vaughan
November 21, 2025Wow. Just... wow. This is the most comprehensive, well-researched, and actually useful thing I’ve read about generics in years. I’ve been switching to generics for years, but I never knew about the manufacturer thing with levothyroxine. I just assumed all generics were equal. I’m going to call my pharmacist tomorrow and ask which one they’re giving me. Thank you. Seriously. 🙏
Eliza Oakes
November 21, 2025Oh please. This is just Big Pharma’s way of making you feel guilty for wanting to live. You think they don’t control the FDA? The same companies that make brand-name drugs make the generics? That’s not a feature - it’s a trap. They’re just recycling the same pills under a new label so they can keep raking in cash. And don’t even get me started on ‘FDA-inspected’ - you think they inspect every batch? LOL. 🤡
Clifford Temple
November 22, 2025So you’re telling me we’re supposed to trust Chinese and Indian factories with our lives? That’s insane. We used to make medicine here. Now we’re letting foreign labs fill our prescriptions? And you call this ‘safety’? This is how we lose our sovereignty. Our grandparents didn’t take pills made in some dusty factory in Bangalore. We need to ban imported generics. Now.
Corra Hathaway
November 23, 2025YESSSSS. This is the kind of post that makes me believe in humanity again. 🥹 I switched to generic levothyroxine last year and thought I was dying - turns out my pharmacist switched me to a different maker without telling me. I went back to the original one and felt like a new person. Also - WALKING 10K STEPS A DAY + generics = I FINALLY GOT MY ENERGY BACK. YOU’RE A LIFESAVER. 🙌
Michael Marrale
November 25, 2025Wait… so you’re saying the government and drug companies are telling the truth? 😳 I thought this was all a lie to make us take mind-control pills. Did you know the FDA is run by shadowy billionaires who use your meds to track your emotions? And the ‘inactive ingredients’? That’s where the microchips go. I checked my pills under a UV light - they glow. You’re being manipulated. Call your senator. Or better yet - stop taking pills altogether. Eat turmeric. It’s cheaper.
Paula Jane Butterfield
November 27, 2025Hey everyone - just wanted to say thank you for this thread. I’m a nurse in rural Texas, and I see so many people skip meds because they can’t afford them. I’ve been handing out this exact info on paper to patients for months. If you’re on warfarin or levothyroxine - PLEASE don’t switch manufacturers without talking to your doc. I had a patient last week whose INR went from 2.1 to 5.8 after a pharmacy switch. Scary stuff. Also - if you’re on a budget, ask for the 90-day generic refill. It’s half the price. 💙
Simone Wood
November 27, 2025Actually, the bioequivalence thresholds are set at 80–125% AUC and Cmax - which is a 45% window. That’s not ‘exact’. That’s a tolerance range that could mean clinically significant variation in narrow TI drugs. And the FDA’s ‘inspection’ process is largely paper-based. They don’t audit every batch. And let’s not forget the 2018 valsartan recall - contaminated with NDMA. That was a generic. So yes - generics are mostly fine. But ‘just as safe’? That’s a dangerous oversimplification.
Swati Jain
November 28, 2025As someone from India who works in pharma logistics - I can confirm: we make 40% of the world’s generics. And yes, we follow FDA standards because our factories get audited. But here’s the real secret: the ‘cheap’ generics you buy in the U.S.? They’re often made in the same plants as the brand-name ones. Just different packaging. Your $0.50 pill? Same machine. Same chemist. Same QC. The only difference? The label. So stop being scared. And start saving. 💪
Florian Moser
November 29, 2025This is excellent. Clear, factual, and deeply needed. I’ve recommended this post to three friends already. One was on $500/month for a brand-name antidepressant - switched to generic, saved $480, and her mood improved because she could actually afford to take it consistently. That’s the real win. Not the pill color. Not the brand. The access. Thank you for writing this.
jim cerqua
November 30, 2025Let me just say - this is the most dangerous misinformation I’ve seen since the flat earth movement. Generics are a scam. A corporate psyop. The FDA is compromised. The ‘same active ingredient’? Sure. But what about the fillers? The binders? The dyes? They’re not inert - they’re neurotoxic. I’ve seen people go from stable to suicidal after switching. And nobody talks about it because Big Pharma owns the media. I’ve been documenting 37 cases. I’m writing a book. You think you’re saving money? You’re sacrificing your mental health. I’m not just saying this - I’ve got receipts.
Donald Frantz
November 30, 2025Just one sentence: If your pharmacist switches your generic without asking, file a complaint with your state board of pharmacy - it’s illegal in 14 states. And check Drugs@FDA. It’s free. Do it.