18 Dec 2025
- 9 Comments
At 65, your bones aren’t just aging-they’re crumbling. One in three women and one in five men over 50 will break a bone because of osteoporosis. And most won’t see it coming. This isn’t just about getting older. It’s about what you’ve done-or didn’t do-for your bones over the last 40 years.
Why Your Bones Are Losing Density
Your bones are alive. They’re constantly being broken down and rebuilt. Up until your late 20s, your body builds more bone than it loses. That’s your peak bone mass. After that, you slowly lose it-about 0.3% to 0.5% per year. But for women, things change fast after menopause. Bone loss can jump to 2% to 3% a year for the first five to seven years. That’s like losing a whole year’s worth of bone in just four months. Men lose bone too, but slower. Why? Women start with less bone mass to begin with, and estrogen-your bone’s best friend-plummets after menopause. Without it, cells that break down bone go into overdrive. Men don’t have that sudden drop, so their bone loss creeps up over decades. But age isn’t the only culprit. Genetics matter. If your mom or dad broke a hip after 50, your risk jumps 60% to 80%. Race plays a role too. White and Asian women are 1.7 times more likely to develop osteoporosis than Black women. That doesn’t mean Black women are immune-it means they’re less likely to be tested or diagnosed early.The Real Danger: Fractures, Not Low Numbers
Doctors measure bone density with a DXA scan. The result? A T-score. Normal is -1.0 or higher. Osteopenia? Between -1.0 and -2.5. Osteoporosis? -2.5 or lower. But here’s the problem: half the people who break bones don’t have osteoporosis on paper. The real warning sign? A past fracture. If you’ve broken a bone from a fall from standing height-or even less-you’re 86% more likely to break another. After a hip fracture, your chance of dying within a year jumps to 20% to 24%. That’s higher than the death rate for many cancers. Dr. Ethel Siris from Columbia University says it plainly: “A single fragility fracture doubles your risk of another.” That’s more powerful than any bone density number. Your body remembers broken bones. So does your risk.What You Can Control: The Big 5 Risk Factors
You can’t change your age or your genes. But you can change these five things:- Calcium: You need 1,000 to 1,200 mg a day. That’s not just milk. It’s yogurt, kale, sardines, fortified tofu. Most people get less than half that. If you’re supplementing, split it into two doses-no more than 600 mg at once. Your body can’t absorb more.
- Vitamin D: If your blood level is under 20 ng/mL, you’re deficient. That’s true for 42% of U.S. adults. You need 800 to 1,000 IU daily. If you’re severely low, you might need 2,000 IU for a few months to catch up. Sunlight helps, but in San Francisco, even in July, you’re not getting enough.
- Smoking: One pack a day increases your fracture risk by 55%. It messes with calcium absorption and lowers estrogen. Quitting doesn’t fix everything overnight, but within a year, your bone loss slows.
- Alcohol: More than two drinks a day? That’s a 41% higher chance of breaking your hip. It affects balance, muscle strength, and bone-making cells.
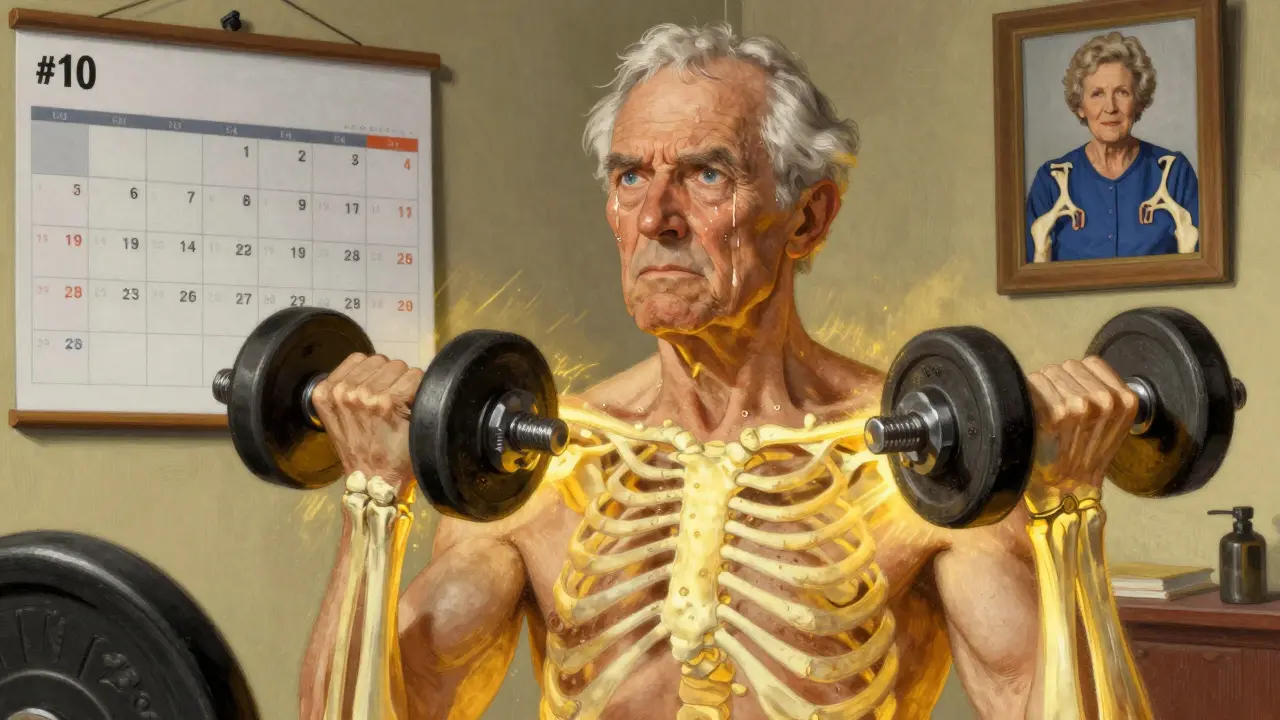
- Sitting: If you don’t move, you lose bone. Sedentary people have 25% to 30% higher fracture risk. Weight-bearing exercise-walking, dancing, stair climbing, lifting weights-builds bone. Resistance training twice a week cuts fracture risk by 30% to 40%.
What’s Not Working: Supplements and Medications
You see ads for calcium pills and bone health gummies. But 68% of people in patient forums say they can’t stick with supplements. Why? Stomach upset. Constipation. Nausea. Many quit after a few weeks. Medications like bisphosphonates (Fosamax, Actonel) help-but 75% of users on Reddit report side effects. GI pain, jaw problems, muscle aches. One in three stops within a year. That’s dangerous. If you’re on these drugs, you need to take them right. You can’t just take them when you remember. There’s a better way. For high-risk patients, new drugs like romosozumab (Evenity) actually build bone instead of just slowing loss. It’s not for everyone-it’s for those with severe osteoporosis or recent fractures. But it shows the field is moving beyond just stopping decay.How to Actually Prevent Fractures
Bone density is only part of the story. Falls are the other half. You can have strong bones, but if you trip and hit the floor, you’re still at risk. Start with your home. Remove loose rugs. Install grab bars in the shower. Add nightlights. Put non-slip mats in the bathroom. These simple steps cut fall risk by nearly 30%. Then, train your balance. Tai chi. Standing on one foot. Heel-to-toe walks. Do it for 10 minutes a day. In a 2022 UK trial, people who did this for six months reduced falls by 45%. Confidence matters. Fear of falling makes you move slower, which makes you more likely to fall. Exercise isn’t optional. It’s medicine. Walk 30 minutes a day, five days a week. Lift weights twice. Squats, lunges, step-ups-anything that makes you work against gravity. You won’t see results in a month. But after six to twelve months, bone density improves. And you won’t fall as easily.
Who Should Get Tested
The U.S. Preventive Services Task Force says: all women over 65. But don’t wait. If you’re over 50 and have any of these, get a DXA scan now:- Broken a bone after 50
- Lost more than 1.5 inches in height
- Been on steroid pills for more than three months
- Have rheumatoid arthritis, type 1 diabetes, or early menopause
- Have a parent who broke a hip
The Long Game: Start Early, Stay Consistent
Professor Cyrus Cooper says it clearly: “Peak bone mass by age 30 determines 60% to 80% of your lifelong risk.” That means your 20s and 30s matter. If you didn’t get enough calcium or exercise then, you’re playing catch-up now. But it’s never too late. Even if you’re 70, starting weight-bearing exercise and getting enough vitamin D can slow loss and reduce falls. The goal isn’t to turn back time. It’s to keep you standing. The cost of ignoring this? $57 billion a year in the U.S. alone. But prevention pays. For every dollar spent on bone health, you save $5.40 in avoided fractures. You don’t need a miracle. You need consistency. Eat your calcium. Move your body. Get your vitamin D. Stop smoking. Cut back on alcohol. Check your home for trip hazards. Talk to your doctor. Don’t wait for a fracture to wake you up.What’s Next?
New research is looking at gut bacteria. Early studies show certain probiotics-like Lactobacillus reuteri-might boost bone density by 1.5% to 2% in a year. Not a cure. But another tool. The WHO just updated its FRAX tool to include time since menopause and fracture healing. That means better predictions. Better care. But the biggest change? We’re starting to treat bone health like heart health. Not just when you’re sick. Every day.Can you reverse osteoporosis naturally?
You can’t fully reverse osteoporosis, but you can stop it from getting worse-and even rebuild some bone. Weight-bearing exercise, adequate calcium and vitamin D, quitting smoking, and avoiding excessive alcohol can slow or halt bone loss. In some cases, especially with new medications like romosozumab, bone density can improve by 5% to 8% over a year. But natural methods alone won’t restore lost bone to normal levels. They’re about prevention and slowing decline.
Is walking enough to improve bone density?
Walking helps, but it’s not enough on its own. Brisk walking is a weight-bearing exercise, which is good-it keeps your bones active. But to build bone, you need resistance too. That means lifting weights, doing squats, lunges, or using resistance bands. Studies show that combining walking with strength training twice a week cuts fracture risk by 30% to 40%. Just walking 30 minutes a day will slow loss, but adding resistance is what builds strength.
Do I need a bone density test if I feel fine?
Yes-if you’re a woman over 65, or a man over 70, or if you’re over 50 and have risk factors like a past fracture, steroid use, early menopause, or a family history of hip fracture. Osteoporosis has no symptoms until you break a bone. By then, it’s too late to prevent damage. A DXA scan is painless, quick, and low-radiation. It’s the only way to know your true bone health.
Can vitamin D alone fix low bone density?
No. Vitamin D helps your body absorb calcium, but it doesn’t build bone by itself. If you’re deficient, fixing that level is essential-but you still need calcium, exercise, and other lifestyle changes. Taking vitamin D without enough calcium won’t improve bone density. Think of it like fuel: vitamin D is the engine, calcium is the gas. You need both.
What foods are best for bone health?
Focus on calcium-rich foods: dairy (milk, yogurt, cheese), canned salmon and sardines (with bones), fortified plant milks, tofu made with calcium sulfate, kale, bok choy, and broccoli. For vitamin D: fatty fish (salmon, mackerel), egg yolks, and fortified foods. Magnesium and vitamin K from nuts, seeds, and leafy greens also support bone. But food alone rarely gives you enough-you may still need supplements to hit daily targets.
Are there alternatives to bisphosphonates?
Yes. For high-risk patients, drugs like romosozumab (Evenity) build new bone and reduce resorption. Denosumab (Prolia) slows bone breakdown. Teriparatide (Forteo) stimulates bone formation. These are used when bisphosphonates aren’t tolerated or aren’t effective. Your doctor will choose based on your fracture risk, medical history, and side effect profile. Lifestyle changes always come first-but medication can be life-saving for those at highest risk.


Mike Rengifo
December 20, 2025Been doing squats and walking daily since I turned 60. My DXA scan last year showed my bone density held steady. No magic pills, just showing up. Still feel like a champ when I lift my grandkid.
Also, no more soda. Switched to sparkling water with lime. Small stuff adds up.
Kitt Eliz
December 20, 2025YESSSS 😤🔥 BONE HEALTH ISN’T A OPTION - IT’S A LIFESTYLE. If you’re not lifting weights by 40, you’re already losing. Calcium? Pfft. You need PROTEIN too - muscle holds bone in place. And vitamin D? If you’re not taking 2000 IU daily in the north, you’re just playing Russian roulette with your hips. 🚫❄️
Also - stop saying ‘I’m too old.’ You’re not. Your habits are. Fix ‘em. Now. 💪🦴
Dominic Suyo
December 22, 2025Let’s be brutally honest - the entire osteoporosis industry is a $57 billion pyramid scheme built on fear and DXA scans.
Half the people diagnosed with ‘osteopenia’ will never fracture a bone. Meanwhile, Big Pharma pushes bisphosphonates like they’re aspirin.
And don’t get me started on ‘Evenity’ - $30,000 a year for a drug that makes your jaw rot? Brilliant. 💸💀
Meanwhile, the real solution? Eat real food. Move. Sleep. Stop being a zombie glued to a chair. But that doesn’t sell ads, does it?
Jedidiah Massey
December 22, 2025As a clinical epidemiologist with 18 years in bone metabolism research, I must emphasize: the T-score is a flawed proxy. The real biomarkers are CTX, P1NP, and bone turnover markers - none of which are routinely measured.
DXA misses microarchitectural deterioration. That’s why fragility fractures occur in ‘osteopenic’ patients.
Also - the 1.5-inch height loss criterion? Underpowered. Spinal compression fractures are often asymptomatic until they’re severe.
And probiotics? L. reuteri ATCC PTA 6475 shows promise in murine models, but human RCTs are still phase II. Don’t overhype.
- J.M., MD, PhD (Harvard, 2008)
Kelly Mulder
December 24, 2025How DARE you suggest that bone density is ‘just’ about calcium and walking? 😳
Have you even read the 2023 Lancet review on epigenetic regulation of osteoblasts? No? Then you’re not qualified to speak.
And vitamin D? You think sunlight in Portland is enough? Please. Your melanin levels are irrelevant - your latitude is the problem. You need D3, not D2. And you need it with K2-MK7, otherwise the calcium goes into your arteries.
And don’t get me started on ‘natural remedies.’ If it’s not FDA-approved, it’s dangerous. Period. 💊🩺
Laura Hamill
December 25, 2025THEY DON’T WANT YOU TO KNOW THIS - BUT THE FDA IS IN BED WITH BIG PHARMA AND THEY’RE HIDING THE TRUTH ABOUT BONES! 😱
They say ‘osteoporosis’ - but what they really mean is ‘government mind control through calcium fear.’
Why do you think they push DXA scans? To track you. To label you. To drug you.
My neighbor’s aunt took Fosamax and lost her teeth. Then she vanished. Coincidence? I think NOT.
Just eat kale. Drink apple cider vinegar. Sleep on a copper mat. That’s the real cure. 💪🌿
Ashley Bliss
December 26, 2025I’ve been thinking about this all night - and I realize… our bones are mirrors of our souls.
When we neglect them, we’re rejecting our own mortality. We’re afraid to age, so we silence the pain with pills and scans.
But true strength isn’t in density - it’s in acceptance.
My grandmother broke her hip at 82 and smiled through it. She didn’t fear the fall - she embraced the fragility.
Maybe the real osteoporosis isn’t in our spines… it’s in our refusal to let go.
So yes - lift weights. Eat kale. But also - forgive yourself. And breathe.
🫶
Emily P
December 27, 2025Quick question - has anyone here tried magnesium glycinate for bone health? I read a small 2021 study that linked it to increased BMD in postmenopausal women, especially when paired with vitamin D. I’ve been taking 400mg daily for 4 months and my muscle cramps stopped… but I’m not sure if it’s helping my bones or just my sleep.
Anyone have data on this? Or just anecdotal?
Janelle Moore
December 27, 2025They told me to take calcium - but I found out the pills are made with crushed seashells from polluted oceans. And the vitamin D? Synthetic. Made in China.
They’re poisoning us slowly. Your bones aren’t weak - your blood is full of toxins.
Do you know how many people die from ‘osteoporosis’ because their kidneys are clogged with fluoride from toothpaste?
Stop trusting doctors. Start detoxing.
Drink lemon water. Sweat in a sauna. And get off the grid. 🌿☢️