28 Dec 2025
- 14 Comments
Every year, thousands of children are at risk of dangerous medication errors-not because of bad intentions, but because pediatric dosing is easy to misread. A prescription that says "10 mL" might look simple, but if the concentration is 80 mg/mL instead of 160 mg/mL, that’s a 2.5x overdose. And if the label doesn’t list the child’s weight in kilograms? You’re flying blind. This isn’t hypothetical. In 2022, the Institute for Safe Medication Practices found that over half of all pediatric medication errors were dosing mistakes. Most of them happened because someone-parent, nurse, even a doctor-didn’t stop to verify the numbers.
Why Pediatric Dosing Is Different
Children aren’t small adults. Their bodies process medicine differently. A dose that’s safe for a 150-pound teen could kill a 20-pound toddler. That’s why every pediatric prescription must be calculated using weight (mg/kg) or body surface area (mg/m²), not just copied from an adult dose. The American Society of Health-System Pharmacists (ASHP) made this official in 2021: no pediatric dose should be given without a weight-based calculation documented in the electronic record.Even small errors matter. A 0.5 mL mistake with a concentrated liquid antibiotic can mean the difference between healing and liver damage. The FDA’s 2023 guidelines say it plainly: all liquid medications for children must show both the amount in milligrams and the volume in milliliters on the label. If it doesn’t? Ask for clarification.
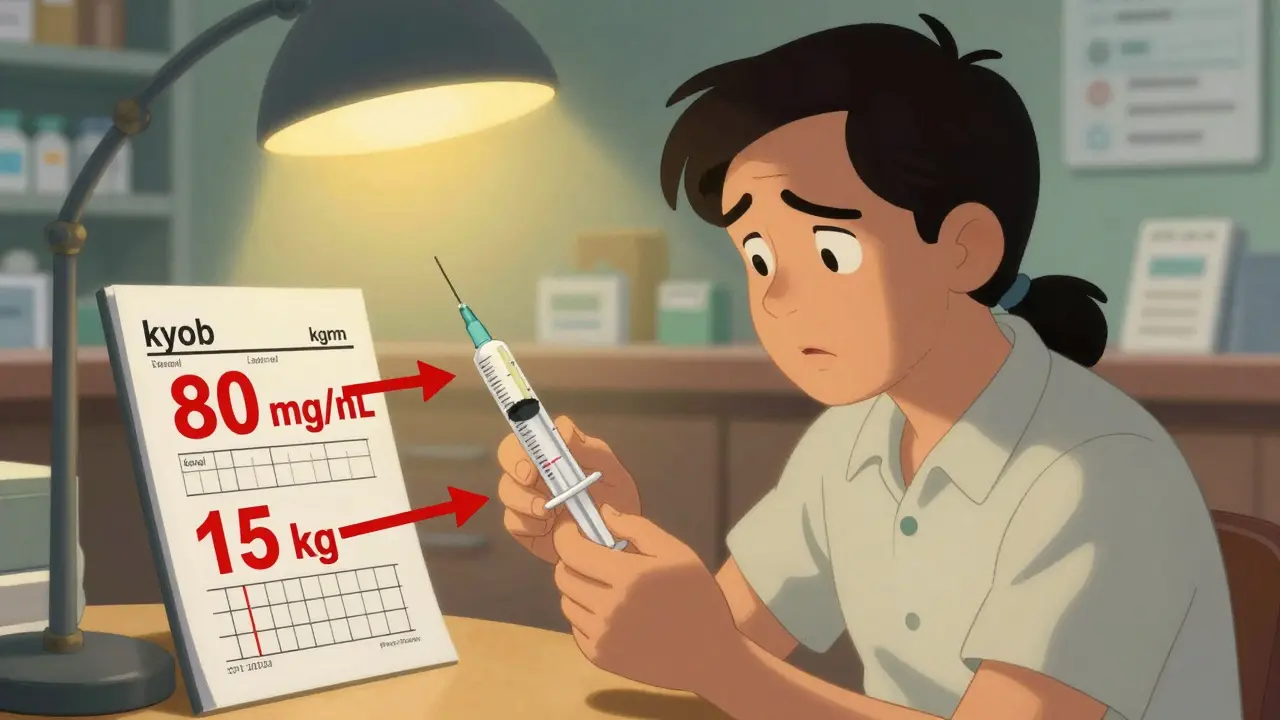
Step 1: Find the Child’s Weight in Kilograms
The first thing you need to check is the weight. Not in pounds. Not in stones. In kilograms. That’s non-negotiable. If the label says "44 lb" but doesn’t convert it to kg, you’re missing half the picture.Here’s the conversion: 1 kg = 2.2 lb. So if your child weighs 33 pounds, divide 33 by 2.2. That’s 15 kg. Simple. But here’s where things go wrong: 18.7% of dosing errors come from messing up this conversion. Some people round 2.2 to 2. That’s a 10% error right there. Always use 2.2 exactly. If the label doesn’t show the kg weight, write it in yourself before giving the medicine.
Step 2: Locate the Dose in Milligrams (mg), Not Milliliters (mL)
Look at the prescription. Does it say "Give 5 mL"? That’s not enough. You need to know how many milligrams are in that 5 mL. That’s the actual amount of drug your child is getting.Concentration is everything. Amoxicillin, for example, comes in different strengths: 40 mg/mL, 80 mg/mL, even 120 mg/mL. If the label says "5 mL of amoxicillin," but doesn’t say the concentration, you could be giving 200 mg or 600 mg-that’s a 3x difference. The CDC found that 37.2% of liquid medication errors in kids under 2 come from this exact confusion.
Always ask: "What is the exact dose in milligrams?" If the pharmacist says "It’s 5 mL," ask again: "But how many mg is that?" Write down both: "200 mg in 2.5 mL of 80 mg/mL solution." That’s the only way to be sure.
Step 3: Check the Dose Against Weight-Based Guidelines
Now you have the child’s weight in kg and the dose in mg. Does it make sense?For common antibiotics like amoxicillin, the standard dose is 40-90 mg/kg/day, split into two or three doses. So if your child is 15 kg, the daily dose should be between 600 mg and 1,350 mg. If the prescription says 1,500 mg per day? That’s high-but possible for a severe infection. If it says 300 mg per day? That’s below the recommended range. Either way, call the doctor. Don’t guess.
For chemotherapy or other high-risk drugs, doctors use body surface area (BSA). The Mosteller formula is the standard: √[height(cm) × weight(kg) / 3600]. You don’t need to calculate this yourself, but you should confirm the label says "dose based on BSA" and includes both height and weight. If it doesn’t, ask for the calculation.

Step 4: Verify the Concentration and Volume Match
Here’s a real example from a 2023 Reddit post: A parent got a prescription for amoxicillin-clavulanate. The label said "10 mL." The doctor meant 200 mg per dose. But the pharmacy dispensed the 80 mg/mL concentration, so 10 mL meant 800 mg-four times the intended dose. The parent noticed the number seemed too high for a 4-year-old and called the pharmacy. They caught it before giving the medicine.That’s why you need to check three things every time:
- The dose in mg (e.g., 200 mg)
- The concentration (e.g., 80 mg/mL)
- The volume to give (e.g., 2.5 mL)
If you multiply concentration × volume, it should equal the dose. 80 mg/mL × 2.5 mL = 200 mg. Perfect. If it doesn’t add up, stop. Call the pharmacy. Don’t assume they made a typo.
Step 5: Use the Right Measuring Tool
Never use a kitchen spoon. Never eyeball it. Always use the syringe or measuring cup that came with the medicine. Those little markings? They’re precise. A household teaspoon holds anywhere from 3-7 mL. That’s a huge range.Pharmacists are trained to give you a device that matches the dose. If they give you a cup for a 1.2 mL dose? That’s a red flag. Ask for a syringe. Syringes are more accurate for small volumes. And if the dose is less than 1 mL, make sure the syringe has 0.1 mL markings.
Also, check the rounding. Some EHR systems like Cerner round doses to make them easier to measure. For example, 150 mg might be rounded to 160 mg if the concentration is 80 mg/mL (so 2 mL instead of 1.88 mL). That’s intentional and safe. But the label should still show the original dose and the adjusted dose. If it doesn’t, ask why.
Step 6: Ask the Three FDA-Recommended Questions
The FDA’s 2023 guide for parents says you should ask these three questions before leaving the pharmacy:- "What is the exact dose in milligrams?" (Not mL)
- "Is this dose appropriate for my child’s current weight?" (They should confirm it matches mg/kg guidelines)
- "Can you show me how to measure this dose with the provided device?" (Watch them do it)
These aren’t just nice-to-haves. They’re your safety net. A 2022 study in BMC Pediatrics found that 43.5% of preventable adverse events in children came from confusion between mg and mL. Asking these questions cuts that risk in half.
What to Do If Something Doesn’t Look Right
You’re not overreacting if you feel uneasy. That’s your instinct working. Here’s what to do:- If the dose seems too high or too low for your child’s size, call the prescribing doctor. Say: "I’m concerned the dose might be off. Can we double-check?"
- If the label doesn’t list weight in kg, ask the pharmacy to correct it. They’re required to do so under FDA guidelines.
- If the concentration isn’t listed, refuse to take it. It’s not safe.
- If you’re still unsure, take the prescription to a second pharmacist. Many hospitals and children’s hospitals have dual verification protocols-why not do the same at home?
One mother in San Francisco caught a 3x overdose on acetaminophen because she compared the label to the manufacturer’s dosing chart. The pharmacy had dispensed the adult concentration (160 mg/5 mL) instead of the children’s (80 mg/0.8 mL). She noticed the volume was way too small for the dose. She called the pharmacy. They apologized. They re-filled it. Her child was fine.
Technology Can Help-But Don’t Rely on It Alone
EHR systems like EPIC and Cerner now have built-in pediatric dose checks. DoseSpot’s AI tool cross-references 15,000+ guidelines and catches 99.2% of errors. Smart pumps and connected scales can auto-verify doses. But these systems aren’t perfect. They can miss a weight entered in pounds instead of kg. They can’t see if you’re using the wrong concentration.Technology is a tool. Your eyes, your questions, and your courage to speak up are the real safety system. Even with AI, the ASHP still requires dual verification for high-risk pediatric doses. That means two people check it. You can be the second set of eyes.
Final Checklist Before Giving Any Pediatric Dose
Before you give your child any medication, run through this quick list:- ✅ The child’s weight is listed in kilograms (kg), not pounds
- ✅ The dose is written in milligrams (mg), not milliliters (mL)
- ✅ The concentration (mg/mL) is clearly printed on the label
- ✅ mg × volume = total dose (e.g., 80 mg/mL × 2.5 mL = 200 mg)
- ✅ The dose falls within standard mg/kg ranges for that drug
- ✅ You’re using the measuring device that came with the medicine
- ✅ You’ve asked the pharmacist to confirm all three FDA questions
If even one item is missing, don’t give the medicine. Call the doctor or pharmacy. It’s better to wait 10 minutes than risk a hospital visit.
Pediatric dosing isn’t complicated. But it demands attention. Every number on that label has a purpose. When you take the time to verify it, you’re not just following rules-you’re protecting your child’s life.
What should I do if the prescription doesn’t list my child’s weight in kilograms?
If the prescription doesn’t include your child’s weight in kilograms, do not fill it until it’s corrected. The American Academy of Pediatrics’ 2024 policy requires all pediatric prescriptions to include weight in kg to prevent conversion errors. Call the prescribing doctor’s office and ask them to update the prescription with the correct weight. If the pharmacy fills it without this, ask them to confirm the dose manually using your child’s weight. Never guess the conversion-always use 1 kg = 2.2 lb exactly.
Can I trust the dose if the label says "as directed"?
No. "As directed" is not acceptable on pediatric prescriptions. This phrase is vague and dangerous. It shifts responsibility away from clear labeling and onto the parent or caregiver to figure out the dose. The FDA and ASHP both require exact dosing instructions for children. If you see "as directed," ask the pharmacist to clarify the exact dose in mg and mL. If they can’t provide it, return to the prescriber. This is a red flag.
Why is it dangerous to use a kitchen spoon to measure liquid medicine?
Kitchen spoons vary widely in size-a teaspoon can hold anywhere from 3 to 7 milliliters. That’s a 130% difference. A dose meant to be 2.5 mL could end up being 5 mL or even 7 mL if you use a spoon. That’s a 100-180% overdose. The American Academy of Pediatrics strongly advises against using household utensils. Always use the syringe, dropper, or cup that comes with the medication. These are calibrated for accuracy and designed specifically for children’s doses.
How do I know if the concentration on the label is correct for my child’s age?
Check the drug’s standard concentration for pediatric use. For example, liquid acetaminophen for children is typically 160 mg/5 mL or 80 mg/0.8 mL. Amoxicillin for kids is often 250 mg/5 mL or 40 mg/mL. If the concentration is unusual-like 120 mg/mL or 200 mg/mL-it’s likely a concentrated formulation for infants or specific conditions. Always ask the pharmacist: "Is this the standard concentration for children?" If it’s not, they should explain why and confirm the dose calculation. Never assume a higher concentration means a higher dose-it’s the mg total that matters.
What should I do if I accidentally give the wrong dose?
If you realize you gave the wrong dose, call Poison Control immediately at 1-800-222-1222. Have the medication bottle, the label, and your child’s weight ready. Do not wait for symptoms to appear. Even small overdoses can be serious in children. If your child is having trouble breathing, is lethargic, vomiting, or having seizures, call 911. Keep the medication bottle with you when you go to the ER. The medical team will need the exact concentration and volume to treat your child properly.

Manan Pandya
December 28, 2025Just read this after my kid got prescribed amoxicillin last week. I didn’t even think to check the concentration-just trusted the pharmacy. Now I’m double-checking every label. Thanks for the clarity.
Nisha Marwaha
December 30, 2025The pharmacokinetic variability in pediatric populations necessitates weight-based dosing paradigms grounded in mg/kg or BSA metrics-this is non-negotiable in clinical pharmacology. Failure to adhere to ASHP 2021 guidelines constitutes a systemic safety lapse, particularly in ambulatory care settings where EHR integration is suboptimal.
Paige Shipe
December 31, 2025I work in a hospital and I’ve seen this so many times. Parents don’t know the difference between mL and mg. It’s not their fault-they’re stressed. But someone needs to be responsible. The system is broken. Why aren’t pharmacies legally required to print the dose in mg on the front of the label? It’s 2024. This shouldn’t be a debate.
Tamar Dunlop
January 1, 2026As a mother of two children who’ve been hospitalized for medication errors, I can say with absolute certainty: this guide is not just helpful-it is life-saving. The emotional toll of nearly losing a child because of a misread concentration is indescribable. Thank you for writing this with such precision and compassion. I will print this and tape it to my medicine cabinet.
David Chase
January 2, 2026USA is the only country where this is even a problem. In Germany, Canada, Australia-they all have standardized pediatric labeling. We’re literally behind the curve. Why are we still letting pharmacies use ‘as directed’? This is why people hate our healthcare system. 🤦♂️💣
Jasmine Yule
January 3, 2026I used to think I was being paranoid when I asked for the mg calculation. Now I know I was just smart. I always ask the three FDA questions now. My daughter’s pediatrician actually praised me for it last week. You’re not overreacting-you’re protecting your kid. Keep doing this.
Greg Quinn
January 4, 2026It’s funny how something so simple-weight in kg, dose in mg-becomes this huge moral test. We’ve turned medicine into a puzzle for parents instead of a system designed for clarity. The real failure isn’t the parent who misreads the label. It’s the system that lets the label be readable in the first place.
Lisa Dore
January 5, 2026I’m a nurse and I’ve seen parents cry because they gave the wrong dose. Please, if you’re reading this-don’t wait until something goes wrong. Ask the questions. Write it down. Use the syringe. You’re not being difficult-you’re being brave. And you’re not alone.
Jim Rice
January 6, 2026Actually, most of these errors happen because parents don’t trust doctors. They read Reddit and then second-guess everything. If the doctor wrote it, it’s fine. Stop overcomplicating. You’re not a pharmacist.
Henriette Barrows
January 8, 2026My 3-year-old had a fever last month and I almost gave him the wrong dose because the label said "5 mL" and I didn’t check the concentration. I called the pharmacy and they were so nice about it. Now I keep a little cheat sheet taped to the fridge. I wish I’d known this before.
Aliza Efraimov
January 9, 2026Here’s the brutal truth: 70% of pediatric dosing errors happen because the weight was entered in pounds instead of kg in the EHR. It’s not the parent’s fault. It’s the system. Pharmacies need to be required to flag any weight entered in lbs and auto-convert it. And if the label doesn’t show mg, it shouldn’t be dispensed. Period.
Kevin Lopez
January 10, 2026mg/kg. BSA. Concentration. Verification. Dual-check. These aren’t suggestions. They’re protocols. If you’re not following them, you’re not practicing medicine-you’re gambling.
Duncan Careless
January 10, 2026Just had to refill my son’s amoxicillin. The pharmacist actually pulled out the syringe and showed me how to measure 1.8 mL. I didn’t even know they still did that. Thank you. I’ll be asking the three questions now. Small things matter.
Samar Khan
January 11, 2026LOL at people stressing over mL vs mg. My cousin’s kid got 10x the dose and they’re fine. Kids are tough. Stop being so paranoid. 😂💊