5 Dec 2025
- 12 Comments
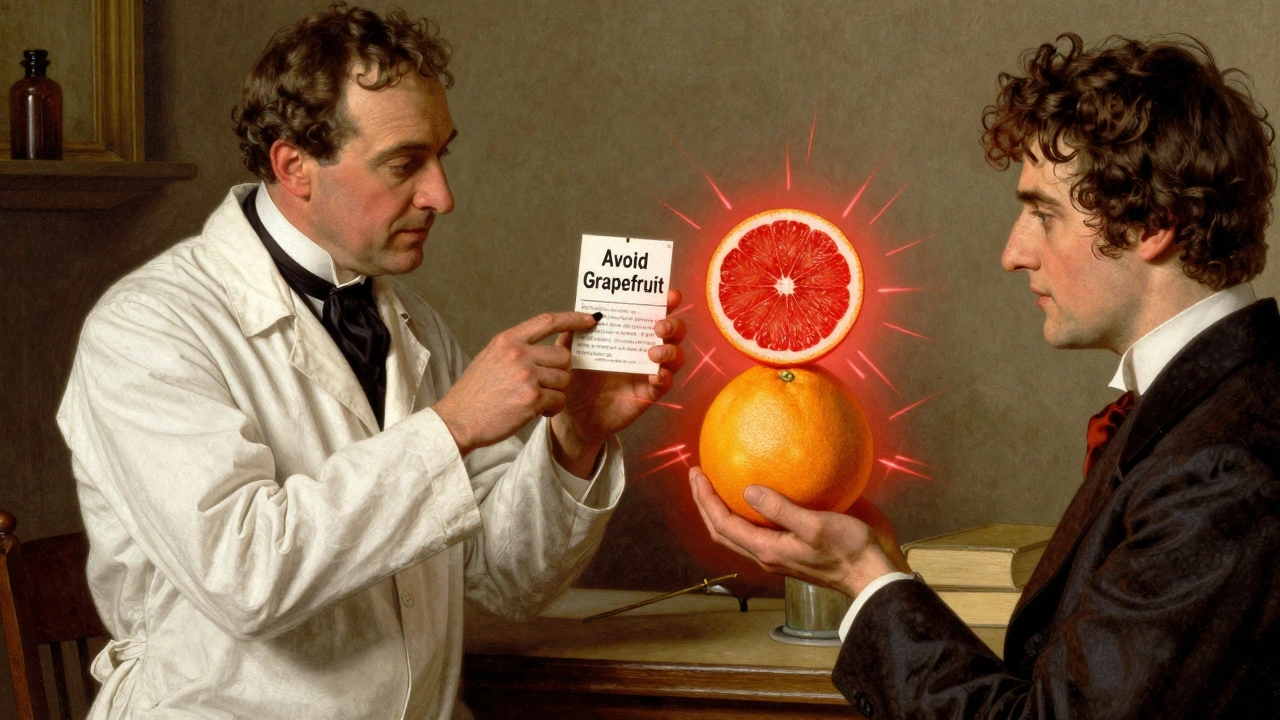
One glass of grapefruit juice in the morning might seem like a healthy start to your day. But if you’re taking certain medications, that juice could be putting your life at risk. This isn’t a myth or a warning from an old wives’ tale-it’s a well-documented, potentially deadly interaction backed by decades of research and confirmed by the FDA, Mayo Clinic, and top medical journals.
How Grapefruit Juice Changes How Your Body Handles Medication
Grapefruit juice doesn’t just mix poorly with some drugs-it actively changes how your body absorbs and processes them. The problem lies in chemicals called furanocoumarins, found naturally in grapefruit, especially in the pulp and peel. These compounds shut down an enzyme in your small intestine called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. When it’s blocked, your body absorbs far more of the drug than it should.
That means a normal dose of your medication can turn into a toxic one. You don’t need to drink a whole pitcher. Just one 200-milliliter glass-about six ounces-can reduce CYP3A4 activity by nearly 50% within four hours. And the effect doesn’t go away after a few hours. It lasts 24 to 72 hours. That’s why even taking your medication at night and drinking grapefruit juice in the morning still puts you at risk.
Which Medications Are Most at Risk?
More than 85 prescription drugs have confirmed interactions with grapefruit juice. But not all are equally dangerous. Some can cause mild side effects. Others can lead to kidney failure, heart rhythm problems, muscle breakdown, or sudden death.
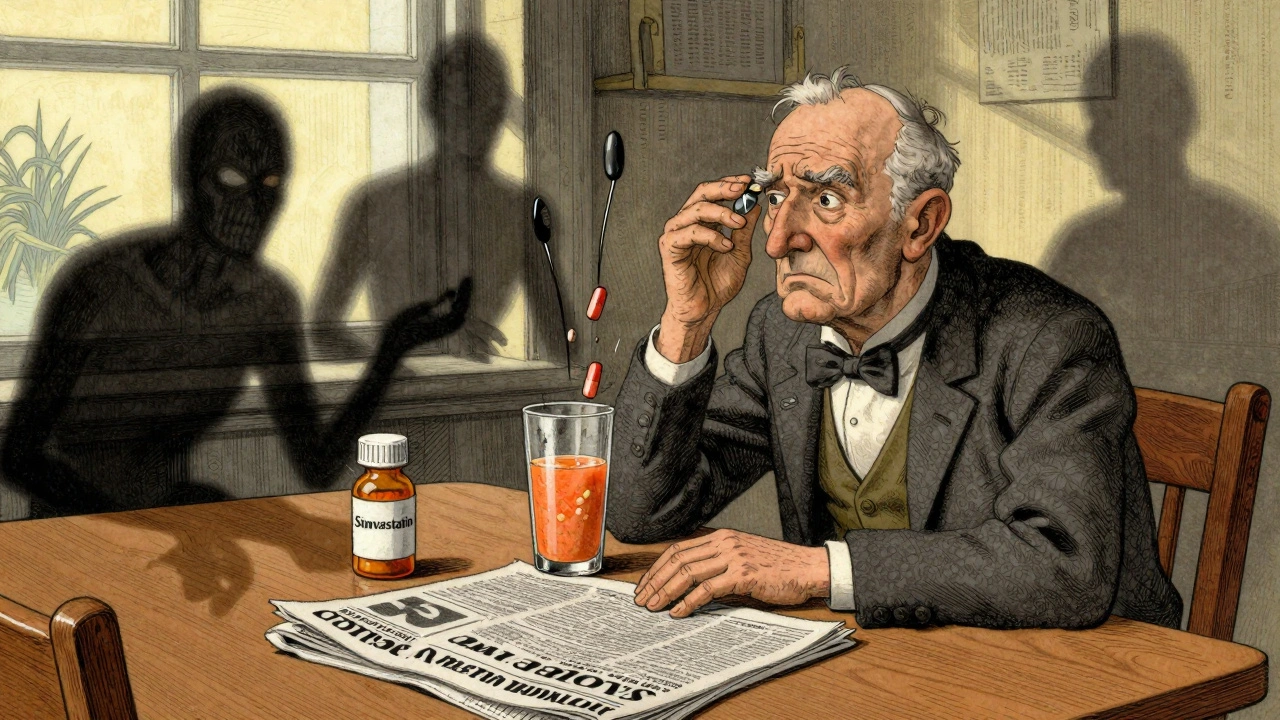
Statins are among the most dangerous. Simvastatin (Zocor) is especially risky. Drinking grapefruit juice while taking it can triple your blood levels of the drug. That raises your risk of rhabdomyolysis-a condition where muscle tissue breaks down and floods your kidneys with toxic proteins. A 2014 study in the Canadian Medical Association Journal found that the risk jumped from 0.04 to 0.44 cases per 100 people per year. That’s a tenfold increase.
Atorvastatin (Lipitor) is less affected, with only a 1.3-fold increase. But pravastatin and rosuvastatin? No interaction at all. If you’re on simvastatin and love grapefruit, talk to your doctor about switching. It’s a simple fix that can save your life.
Calcium channel blockers used for high blood pressure also react badly. Felodipine (Plendil) can see a fivefold increase in blood levels. Nifedipine (Procardia) jumps by 3.3 times. But amlodipine (Norvasc)? Almost no effect. Again, the difference matters. Your doctor can often switch you to a safer alternative without losing blood pressure control.
Immunosuppressants like cyclosporine (Neoral) are another high-risk group. Grapefruit juice can boost cyclosporine levels by 50-60%. For transplant patients, that means higher chances of kidney damage, infection, or rejection. Even small changes in these drug levels can be catastrophic.
Antiarrhythmics like amiodarone (Cordarone) can cause dangerous heart rhythms if grapefruit juice pushes levels too high. And drugs like trazodone and zolpidem? They’re generally safe. But you can’t assume. You have to check.
It’s Not Just Grapefruit Juice
Don’t think swapping to orange juice solves the problem. Seville oranges-used in traditional marmalade-and pomelos contain the same furanocoumarins. So if you’re on a high-risk medication, skip those too.
But sweet oranges (like navel or Valencia), tangerines, and lemons? Safe. They don’t contain the chemicals that cause the interaction. You can enjoy them without worry.
Why This Interaction Is So Hard to Predict
Not everyone reacts the same way. Some people absorb way more of the drug after drinking grapefruit juice. Others barely see a change. Why? Because CYP3A4 enzyme levels vary from person to person. People with naturally high levels in their intestines get hit hardest. But there’s no test to measure this. No blood work can tell you if you’re at risk.
That’s why experts say the only safe approach is to avoid grapefruit entirely if you’re on a medication that interacts with it. Even if you’ve had it before without problems, your body changes. Your liver, your kidneys, your other meds-they all shift over time. What was safe last year might be dangerous this year.
What You Should Do Right Now
Step one: Look at your medication list. Not just prescriptions-include over-the-counter drugs and supplements. Some antihistamines like fexofenadine (Allegra) interact too. So do certain anti-anxiety meds and erectile dysfunction pills.
Step two: Check the label. Since 2014, the FDA has required drug manufacturers to include grapefruit warnings on packaging for affected medications. If it says “avoid grapefruit,” take it seriously.
Step three: Talk to your pharmacist. Pharmacists are trained to spot these interactions. A 2021 study found 89% of community pharmacists routinely check for grapefruit interactions when filling prescriptions. Ask them directly: “Does this medicine interact with grapefruit?” Don’t assume they’ll bring it up.
Step four: Keep a written list of all your medications and supplements. Bring it to every appointment. Many patients don’t remember all the pills they take-especially older adults, who are the most likely to be on multiple drugs and drink grapefruit juice daily. According to USDA data, 40% of grapefruit consumers are over 65. That’s a dangerous overlap.
What If I Can’t Give Up Grapefruit?
Some people love grapefruit. They eat it for breakfast every day. They’ve done it for years. But if you’re on a high-risk medication, there’s no safe amount. No “just a little.” The interaction is irreversible and long-lasting. One glass today can affect your meds for three days.
Your best option? Talk to your doctor about switching medications. For statins, switch from simvastatin to pravastatin or rosuvastatin. For blood pressure, swap felodipine for amlodipine. For immunosuppressants, consider tacrolimus instead of cyclosporine. These alternatives work just as well-with no grapefruit risk.
And if you’re not on a high-risk drug? Then you’re probably fine. But don’t guess. Check.
The Bigger Picture: Why This Isn’t Common Knowledge
Despite decades of research, patient awareness is shockingly low. A 2022 survey by the National Community Pharmacists Association found only 38% of patients recalled being warned about grapefruit interactions when prescribed affected medications. That’s not just a gap in communication-it’s a public health blind spot.
Drug companies have lost over $1.2 billion in annual sales because people quit taking simvastatin just to avoid grapefruit. But that’s not the real cost. The real cost is the preventable hospitalizations, kidney failures, and deaths that happen because someone didn’t know.
There’s hope on the horizon. In October 2023, the USDA announced CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety trials. Eventually, we may have a safe version. But that’s years away. Until then, the rules haven’t changed.
Bottom Line: When in Doubt, Skip It
Grapefruit juice is not the enemy. It’s full of vitamin C, antioxidants, and fiber. But when it meets certain medications, it becomes a silent danger. You can’t feel it. You can’t see it. You might not even notice until it’s too late.
If you take any prescription drug, ask one simple question: “Does this interact with grapefruit?” If the answer is yes, avoid it completely. No exceptions. No compromises. Your body doesn’t have a warning system for this. Your doctor and pharmacist do. Use them.
It’s not about giving up a healthy habit. It’s about protecting your life. And sometimes, the safest choice is the simplest one: skip the grapefruit juice and grab an orange instead.

pallavi khushwani
December 6, 2025So I’ve been drinking grapefruit juice with my statin for years and never had an issue. But now I’m wondering if my body just hasn’t caught up to the betrayal yet. Maybe my CYP3A4 is lazy. Or maybe I’m just lucky. Either way, I’m switching to oranges tomorrow. Better safe than sorry, right?
Dan Cole
December 6, 2025You’re not lucky-you’re statistically overdue. The enzyme inhibition is dose-independent and cumulative. The fact that you haven’t experienced rhabdomyolysis yet doesn’t mean it’s not happening at a subclinical level. Your creatine kinase is probably elevated right now and you’re too oblivious to notice. This isn’t luck. It’s impending biological reckoning.
Billy Schimmel
December 7, 2025Wow. So basically, the universe is saying ‘no grapefruit’ and we’re all just arguing about it like it’s a Netflix show. I’ll just stick with orange juice and pretend I’m a normal person.
Kay Jolie
December 9, 2025Let’s be real-the CYP3A4 enzyme isn’t just some passive bystander. It’s the gatekeeper of your pharmacokinetic kingdom, and grapefruit juice? It’s the anarchist with a molecular crowbar. The fact that we’re still allowing this interaction to fly under the radar is a travesty of pharmaceutical negligence. I mean, do we really need another 1.2 billion dollars in lost sales before the FDA mandates grapefruit-free labeling on every prescription bottle? It’s not just about safety-it’s about dignity.
Shayne Smith
December 9, 2025I just read this while sipping my grapefruit juice. And now I’m staring at my bottle of Lipitor like it’s a ticking bomb. Thanks for the existential dread before coffee.
Max Manoles
December 9, 2025It’s fascinating how the same biochemistry that makes grapefruit juice dangerous also makes it a potent antioxidant. Evolution didn’t intend for humans to take synthetic drugs, so the interaction is just nature’s way of saying, ‘You’re doing this wrong.’ The real tragedy isn’t the juice-it’s that we’ve outsourced our health to pills and then blame the fruit.
Rashmi Gupta
December 9, 2025Actually, the FDA warning only applies to 85 drugs. But there are over 2000 drugs on the market. So if you’re not on one of those 85, you’re fine. Also, grapefruit juice is a superfood. You’re overreacting.
Kumar Shubhranshu
December 10, 2025Stop drinking grapefruit juice if you’re on meds. Simple. No debate. I’ve seen people die from this. You’re not special.
Karen Mitchell
December 11, 2025This article is dangerously irresponsible. It implies that patients are incapable of making informed decisions. Why not just ban grapefruit entirely? Or better yet, force everyone to take genetic tests for CYP3A4 expression before prescribing any drug? This is medical paternalism dressed up as public health advice.
olive ashley
December 13, 2025Let me guess-this is all a Big Pharma plot. They want you to stop eating grapefruit so you’ll buy more expensive statins. And those CRISPR grapes? Totally fake. The USDA is in on it. They’ve been spraying nano-chips in citrus since 2018. I know someone who works at a lab in Florida. They’re testing them on cats. Cats are the control group.
Ibrahim Yakubu
December 15, 2025Back home in Nigeria, we don’t even have grapefruit. We have oranges, limes, and pawpaw. And our people don’t die from statins. Why? Because we don’t trust Western medicine. We use herbs. And our ancestors knew what they were doing. You think a fruit can kill you? You’re weak.
Mansi Bansal
December 15, 2025It is, without a doubt, an egregious oversight in contemporary pharmacological education that the general populace remains so woefully uninformed regarding the biochemical antagonism between furanocoumarins and the cytochrome P450 enzyme system. The societal implications are profound: a public health crisis concealed beneath the veneer of a breakfast beverage. One must question the efficacy of current regulatory dissemination mechanisms, particularly when the mortality risk is quantifiably elevated by an order of magnitude. The onus, therefore, rests not solely upon the patient, but upon the entire medical-industrial complex to ensure unequivocal, unambiguous, and universally accessible communication of such risks. To neglect this duty is not merely negligence-it is a moral abdication.