7 Feb 2026
- 12 Comments
When a doctor hands you a prescription for a generic drug, you might not think much about it. But what if that same doctor says nothing at all? Or worse, says something like, "This might not work as well, but it’s cheaper"? That one moment - or lack of moment - can change whether you take the medicine, stick with it, or stop cold because you’re convinced it won’t work. The truth is, clinician communication doesn’t just inform patients about generics - it shapes whether they believe in them.
Let’s be clear: generic drugs aren’t second-rate. They’re the same as brand-name drugs in active ingredients, strength, dosage form, and how they work in the body. The FDA requires them to be within 80-125% bioequivalent to the brand. That’s not a guess. It’s science. But patients don’t always know that. And when they don’t, they listen to what their doctor or pharmacist says - or doesn’t say.
Communication isn’t optional - it’s clinical
A 2011 study of nearly 2,000 patients found something startling: the biggest factor influencing whether someone took a generic drug wasn’t cost, wasn’t brand loyalty, and wasn’t even how safe they thought it was. It was whether their clinician talked to them about it. Patients who got even a brief explanation were 37% more likely to stick with the generic. That’s not a small difference. That’s the difference between a drug working and not working - because if you don’t take it, it doesn’t matter how good it is.
Think about it this way: if your doctor prescribes a new pill and says, "This is a generic version of your old one," without explaining what that means, you’re left to fill in the blanks. And your brain will fill them with fear. Maybe you’ve heard stories. Maybe you’ve seen a different-colored pill and assumed something changed. Maybe you’re worried it won’t control your blood pressure or your seizures like the brand did. Those fears aren’t irrational - they’re human. And they’re amplified when no one addresses them.
What good communication actually sounds like
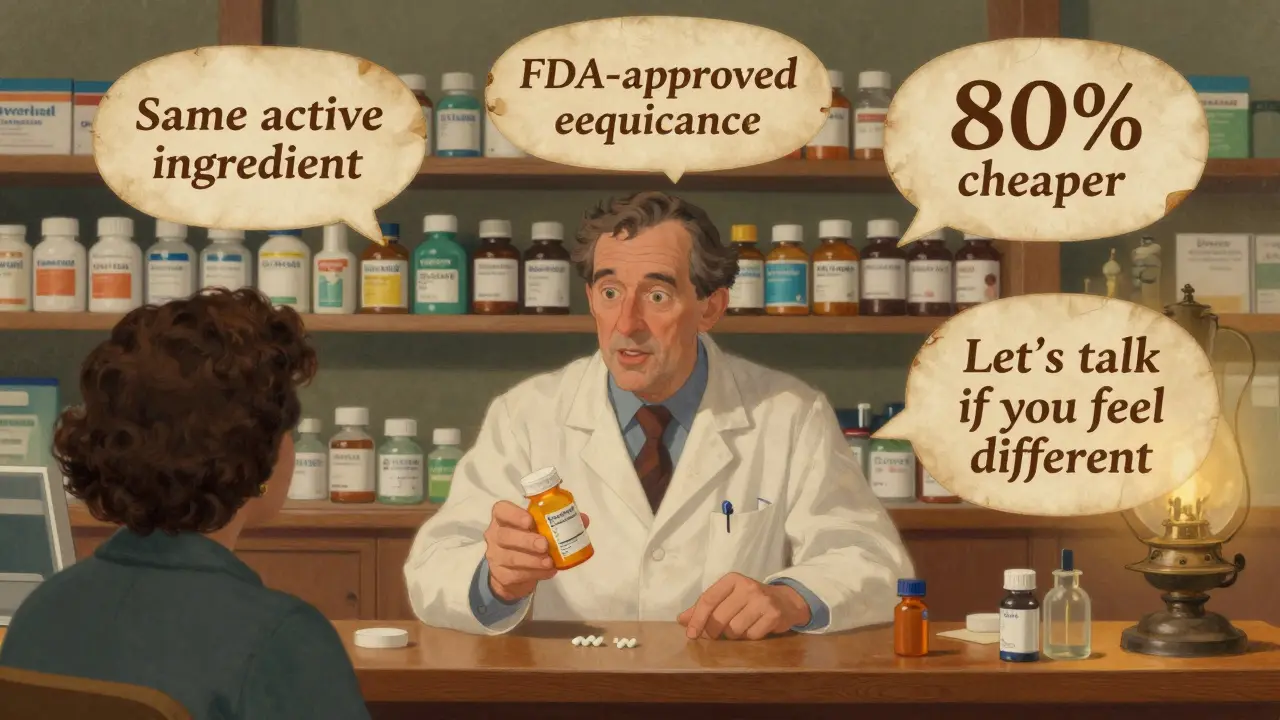
Not all conversations about generics are created equal. Some just say, "We’re switching you." Others make a real difference. Research shows the most effective communication includes four clear elements:
- "This generic has the same active ingredient as your brand-name drug." - No jargon. Just facts.
- "The FDA requires it to work the same way - within 80-125% of the brand." - This number matters. It’s not a vague promise. It’s a standard.
- "It costs about 80-85% less." - People understand money. Saying this isn’t about saving the system - it’s about saving them.
- "Some people worry they’ll feel different. That’s normal. But if you feel worse, let’s talk - it might not be the drug." - This is the game-changer. It’s called managing the nocebo effect.
The nocebo effect? It’s the flip side of the placebo effect. If you expect side effects, your body can start showing them - even if the drug is identical. A 2019 JAMA study found patients who were told upfront that generics are safe and identical reported 28% fewer side effects after switching than those who got a generic with no explanation. The drug didn’t change. Their expectations did.
Who’s being left behind - and why
Communication gaps aren’t equal across all patients. A 2016 NIH survey showed non-Caucasian patients were 1.7 times more likely to distrust generics. Patients earning under $30,000 a year were 2.3 times more likely to insist on brand-name drugs. Why? Because trust isn’t just about information - it’s about culture, history, and experience.
One patient in a 2023 Reddit thread described how her cardiologist spent 10 minutes showing her FDA data, saying he takes generics himself, and even explained why the shape and color changed. She’s been on it for two years with zero issues. Another patient on Healthgrades said her pharmacist handed her a new pill, then said, "Some people react to generics." She stopped taking it for three weeks. One conversation. One word. One moment of poor communication - and a treatment failed.
Studies analyzing over 4,200 patient reviews found that 78% of positive experiences mentioned clinician communication as the reason they trusted the generic. Eighty-nine percent of negative experiences blamed poor or absent communication. That’s not coincidence. That’s cause and effect.
The cost of silence
Generics make up 90% of all prescriptions filled in the U.S. But they account for only 23% of drug spending. That’s $37 billion saved every year. Yet, brand-name preference requests have climbed from 12% in 2010 to 23% in 2022. Why? Because people aren’t being told the truth - or they’re being told the wrong thing.
Only 38% of physicians and 52% of pharmacists consistently talk to patients about generics. Even fewer know the exact FDA bioequivalence range. In one 2019 survey, only 54% of doctors got the number right. How can you explain something you don’t fully understand?
And time? The average clinician spends just 1.2 minutes per patient on this topic. That’s not enough. But it doesn’t have to be more. The American Pharmacists Association created a 15-minute training module that cut communication time by 38% while boosting patient understanding from 42% to 87%. The secret? Scripts. Structure. Clarity.

What’s changing - and what’s next
Change is coming. In 2024, Epic Systems launched the "Generic Confidence Score," a tool built into electronic health records that reminds clinicians to cover the four key points before switching a patient. The FDA now offers patient materials in 12 languages. Medicare is starting to tie reimbursement to how well providers explain generics. And by 2025, the CDC plans to make generic communication part of national health literacy standards.
But the biggest opportunity isn’t technology - it’s training. Clinicians need to stop seeing this as a paperwork task. It’s a clinical intervention. It’s as important as prescribing the right dose. A patient who believes in their medication is more likely to take it, stick with it, and get better. A patient who doubts it? They’ll stop. And that’s not just a missed dose - it’s a missed outcome.
It’s not about the pill - it’s about the promise
Generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t need to spend millions on ads or patents. The science is solid. The data is clear. The savings are real.
But none of that matters if the person holding the prescription doesn’t believe it. And that’s where you - the doctor, the pharmacist, the nurse - come in. You’re not just handing out pills. You’re handing out trust. And trust? It’s built one conversation at a time.
Why do some patients think generic drugs are less effective?
Patients often believe generics are less effective because of misinformation, lack of explanation, or past experiences with poorly made generics (which are rare today). Brand-name marketing has long implied superiority, and without clear communication from clinicians, patients fill the gaps with assumptions. Studies show that when providers explain FDA bioequivalence standards and confirm identical active ingredients, skepticism drops sharply.
Can a doctor legally refuse to prescribe a generic?
Yes, but only if they write "Do Not Substitute" on the prescription. This is typically done for drugs with narrow therapeutic windows - like epilepsy or thyroid medications - where even small differences matter. However, most generics are fully equivalent. The FDA requires all generics to meet the same strict standards as brand-name drugs. Refusing a generic without medical justification often stems from patient preference or clinician bias, not science.
How do I know if a generic is truly equivalent to the brand?
The FDA requires generics to prove bioequivalence: they must deliver the same amount of active ingredient into the bloodstream within 80-125% of the brand-name drug’s rate. This is tested in clinical trials with healthy volunteers. The FDA also inspects manufacturing facilities - same as for brand-name drugs. You can check the FDA’s Orange Book online (or ask your pharmacist) to confirm therapeutic equivalence codes (AB-rated means fully substitutable).
What should I say if a patient complains about side effects after switching to a generic?
First, don’t dismiss it. Ask what they’re feeling - headaches? Fatigue? Dizziness? Then explain that while the active ingredient is identical, inactive ingredients (like fillers or dyes) can differ. These rarely cause issues, but some people are sensitive. If symptoms persist, consider switching back temporarily - not because the generic is inferior, but to rule it out. Often, symptoms fade as expectations shift. Document the conversation. Reassure them you’re listening - and that you’ve seen this before.
Are there any generics that aren’t safe?
The FDA approves over 10,000 generic drugs each year, and nearly all are safe and effective. Rare cases of problems - like the 2012 bupropion recall - were due to manufacturing flaws, not the generic model itself. These are investigated and corrected. Today’s generics are held to the same standards as brand-name drugs. The real risk isn’t the generic - it’s the lack of communication. Patients who aren’t told why a generic is safe are more likely to stop taking it, which increases health risks far more than the drug itself.
Looking ahead, as more complex generics - like inhalers and injectables - enter the market, communication will become even more critical. Patients won’t just need to understand the drug. They’ll need to understand the process. And that starts with you.


PAUL MCQUEEN
February 7, 2026Wow. So let me get this straight - we’re now treating patients like toddlers who need a PowerPoint presentation just to take a pill? Next they’ll need a signed consent form before they can breathe oxygen.
Chelsea Deflyss
February 8, 2026i read this and thought 'wow this is so true' but then i remebered my doc just handed me a pill and said 'take this' and i did. no explaination needed. people are tooo sensitive these days.
Random Guy
February 9, 2026soooo... doctors are now pharmacists? nurses? therapists? i get it, we want people to take meds. but this is like asking a mechanic to explain why your car doesn’t make a noise when you press the gas pedal. some people just wanna drive, not take a college course on combustion engines.
Brett Pouser
February 11, 2026I’m from the South and I’ve seen this firsthand. My grandma refused her blood pressure med for six months because the pill was a different color. She said, 'It don’t look right, boy.' So I sat her down, showed her the FDA sticker, told her my cousin takes the same one. She’s been on it two years now. No issues. It’s not about the science - it’s about the handshake.
Andrew Jackson
February 12, 2026The erosion of clinical authority is a direct consequence of the democratization of medical knowledge. When patients are empowered with Google searches and Reddit anecdotes, the very foundation of physician-patient trust is undermined. The FDA’s bioequivalence parameters are not negotiable; they are the product of rigorous, peer-reviewed, statistically significant methodology. To reduce this to a marketing campaign is not merely misguided - it is an affront to evidence-based medicine.
MANI V
February 12, 2026This is why America is crumbling. You people treat medicine like a customer service call. 'Oh, I don’t trust this pill because it’s cheaper!' What about the billions we send overseas to manufacture insulin? The same factories? The same inspectors? The same FDA oversight? You’re letting fear override logic because you’d rather believe in conspiracy than in science. Your distrust isn’t informed - it’s performative.
Tricia O'Sullivan
February 13, 2026I work in a rural Irish pharmacy. We see this every day. An elderly man refuses his generic statin because it’s 'not the blue one.' We show him the leaflet, explain the AB rating, offer to call his GP. He takes it. No drama. No panic. Just clarity. It’s not about time - it’s about intention. A few calm words, delivered with dignity, do more than any pamphlet.
Tasha Lake
February 14, 2026The nocebo effect is such a fascinating neurobiological phenomenon - it’s essentially a top-down modulation of somatic perception via expectation encoding in the anterior cingulate and insular cortices. When clinicians fail to reframe the patient’s cognitive schema around bioequivalence, you’re essentially priming the HPA axis to generate iatrogenic symptoms. The 28% reduction in reported side effects? That’s not placebo. That’s neurocognitive reattribution. We need to train clinicians in cognitive behavioral reframing techniques, not just script delivery.
Susan Kwan
February 15, 2026I’m a nurse. I’ve watched patients cry because they think the generic 'isn’t strong enough.' I’ve seen people stop their seizure meds because the pill was a different shape. This isn’t about education. It’s about trauma. Many of these patients were lied to by pharma ads for years. Now they’re being told to 'trust the system.' But the system broke their trust first. So yes - talk to them. But don’t just hand them a script. Listen. Then speak.
Karianne Jackson
February 15, 2026i had a friend who stopped her anxiety med because it was a white pill instead of blue. she said 'it felt like a different person.' i told her that’s dumb. she said 'you don’t get it.' she’s still off it. and now she’s in therapy. and i’m just over here wondering why we’re all so scared of a little white pill.
Alex Ogle
February 17, 2026I’ve been in this game for 22 years. I’ve seen patients switch from brand to generic and swear they felt worse. Then we do a double-blind switch - same pill, different color, same dose. They say 'this one’s better.' The drug didn’t change. Their brain did. That’s the real clinical challenge. We treat the body. But the mind? That’s the wild frontier. And if we don’t speak to it - really speak - we’re not healing. We’re just handing out candy with a label.
Tom Forwood
February 18, 2026yo i work at a clinic in ohio and we started using a 30-second script: 'same drug, same results, 80% cheaper. if you feel weird, tell us. but it’s probably your brain being weird.' we cut refill failures by 40%. no one’s mad. no one’s confused. just simple. real. human. the docs thought it was too casual. turns out patients like it when you talk like a person, not a textbook.