16 Feb 2026
- 0 Comments
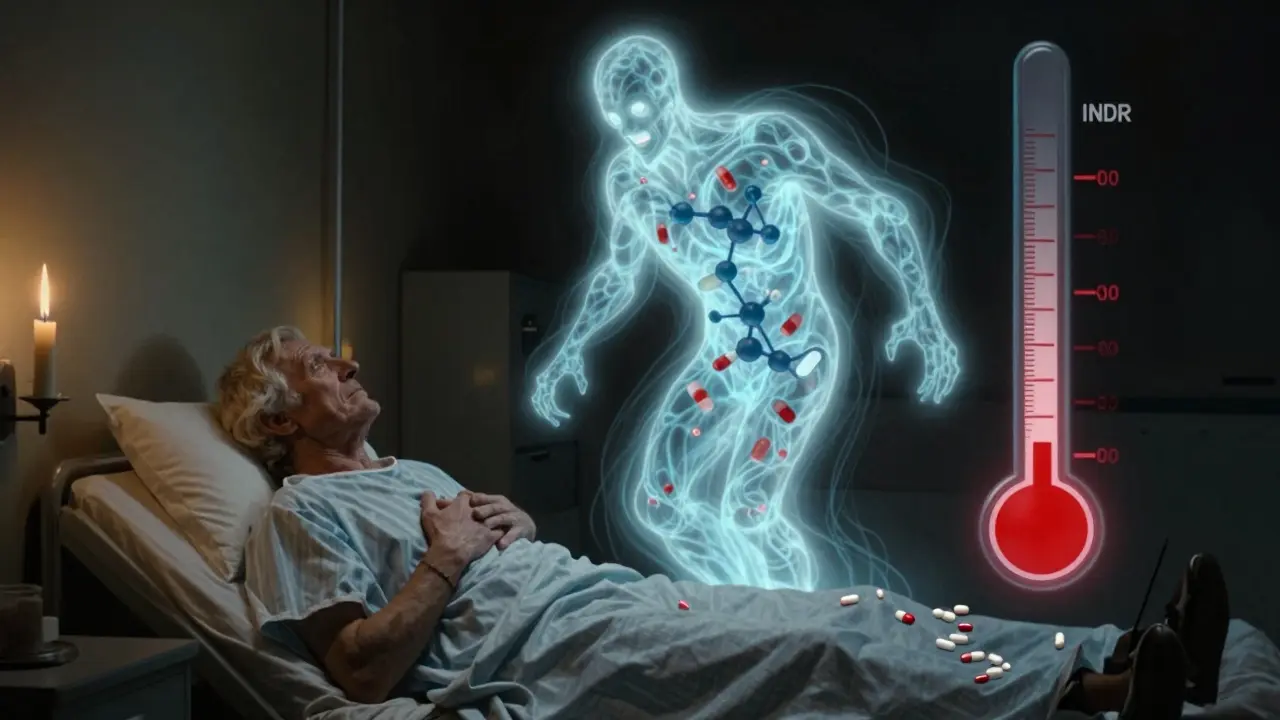
Warfarin-TMP-SMX INR Risk Calculator
Calculate Your Risk
EMERGENCY WARNING: If INR exceeds 5.0 or you experience bleeding symptoms (unusual bruising, blood in urine/stool, headaches, dizziness), seek immediate medical attention.
When you're on warfarin, even a simple antibiotic can turn dangerous. Take trimethoprim-sulfamethoxazole - commonly known as Bactrim or Septra. It's often prescribed for urinary tract infections, sinus infections, or pneumonia. But if you're taking warfarin to prevent clots, mixing these two can send your INR sky-high, putting you at serious risk of internal bleeding. This isn't a rare side effect. It's a well-documented, predictable, and often deadly interaction that happens more often than most people realize.
Why This Interaction Happens
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It's a delicate balance. Too little, and you bleed. Too much, and you clot. The drug itself is a mix of two forms: S-warfarin and R-warfarin. The S-form is three to five times stronger at thinning your blood. And it's mostly broken down by one liver enzyme: CYP2C9. Trimethoprim-sulfamethoxazole messes with this system in three ways. First, trimethoprim blocks CYP2C9. That means your body can't clear S-warfarin the way it should. The drug builds up. Second, sulfamethoxazole pushes warfarin off proteins in your blood. Since warfarin is 97-99% bound to albumin, even a small displacement can flood your system with free, active drug. Third, the antibiotic kills off some of your gut bacteria that naturally make vitamin K. Less vitamin K means warfarin works even harder. The result? INR doesn't just creep up - it spikes. Studies show that within 36 to 72 hours of starting TMP-SMX, INR levels jump an average of 1.8 units. For someone with a stable INR of 2.5, that’s a jump to 4.3 - a level where bleeding risk increases sharply.How Dangerous Is It?
An INR above 4.0 is already considered high risk. Above 5.0? That’s a red zone. The American Heart Association says the chance of serious bleeding - like a brain bleed or gastrointestinal hemorrhage - rises dramatically at these levels. In one study of over 70,000 warfarin users, TMP-SMX was linked to 88% more cases of elevated INR than expected by chance alone. Real-world cases are terrifying. A 78-year-old man with a mechanical heart valve had his INR hit 8.2 after three days of Bactrim. He nearly bled out. A nurse practitioner reported multiple elderly patients going from INR 2.5 to 6.0 within 72 hours. The FDA has logged over 1,800 reports of this interaction over five years. Nearly half led to hospitalization. Almost 4% were fatal. Not everyone reacts the same. Men are 9% more likely than women to have a dangerous rise in INR. Older adults, especially those over 75, are at higher risk. People with liver disease, heart failure, or poor nutrition are also more vulnerable. Their bodies handle the drug imbalance less well.How It Compares to Other Antibiotics
Not all antibiotics are created equal when it comes to warfarin. TMP-SMX is one of the worst offenders.- Trimethoprim-sulfamethoxazole: Increases INR by 1.8 units on average
- Ciprofloxacin (a fluoroquinolone): Increases INR by 0.9 units
- Amoxicillin: Increases INR by just 0.4 units

What Doctors Should Do
Experts agree: avoid TMP-SMX if possible. The American College of Chest Physicians says to choose a different antibiotic unless there’s absolutely no alternative. For a urinary tract infection, nitrofurantoin is often a safer pick. For pneumonia, doxycycline or azithromycin may work better. But if TMP-SMX is the only option? Then you need a strict plan:- Check INR before starting the antibiotic.
- Check INR again within 48 to 72 hours - don’t wait.
- Reduce the warfarin dose by 20-30% as a precaution, especially in older patients or those with other risk factors.
- Monitor INR every 3-4 days while on the antibiotic.
What to Do If INR Goes Too High
If INR is between 4.0 and 5.0 and there’s no bleeding, skip 1-2 doses of warfarin. Resume at a lower dose. If INR is above 5.0 with minor bleeding - like bruising, nosebleeds, or blood in urine - give 1-2.5 mg of oral vitamin K. It reverses warfarin’s effect over 24-48 hours. If INR is over 10 or there’s serious bleeding - vomiting blood, a head injury, or sudden weakness - you need emergency treatment: 5-10 mg of IV vitamin K plus a clotting factor concentrate. Fresh frozen plasma or 4-factor prothrombin complex concentrate can stop the bleeding fast.