13 Feb 2026
- 14 Comments
When you have COPD, your lungs aren’t the only thing suffering. Many people don’t realize that sarcopenia-the loss of muscle mass and strength-is a common and dangerous side effect. In fact, about 1 in 5 people with COPD develop it. And when they do, their chances of dying within five years drop from 45% to as low as 27%. That’s not just about feeling weak. It’s about losing the ability to walk, climb stairs, or even get out of bed without help. The good news? This isn’t inevitable. With the right nutrition and targeted resistance training, you can rebuild muscle, reduce hospital visits, and take back your independence.
Why Sarcopenia Hits Harder in COPD
Sarcopenia isn’t just aging. In COPD, it’s accelerated. While healthy older adults lose about 1-2% of muscle each year, people with COPD lose up to 3.2%. Why? It’s not one thing-it’s a perfect storm. Constant inflammation from lung damage floods the body with chemicals like TNF-α and IL-6 that break down muscle. Low oxygen levels during sleep, especially if your oxygen saturation drops below 88% for more than 30% of the night, directly damage muscle tissue. And because breathing is so hard, many people avoid movement. Less movement means faster muscle loss.
What’s worse? The muscles that matter most aren’t just your legs. In COPD, the muscles in your chest-especially the pectoralis major-are often the first to shrink. One study found 68% of COPD patients had significant chest muscle loss, compared to only 22% of healthy people their age. That’s not just about looking weaker. It’s about losing the ability to take a full breath. Your diaphragm and rib cage muscles need strength too.
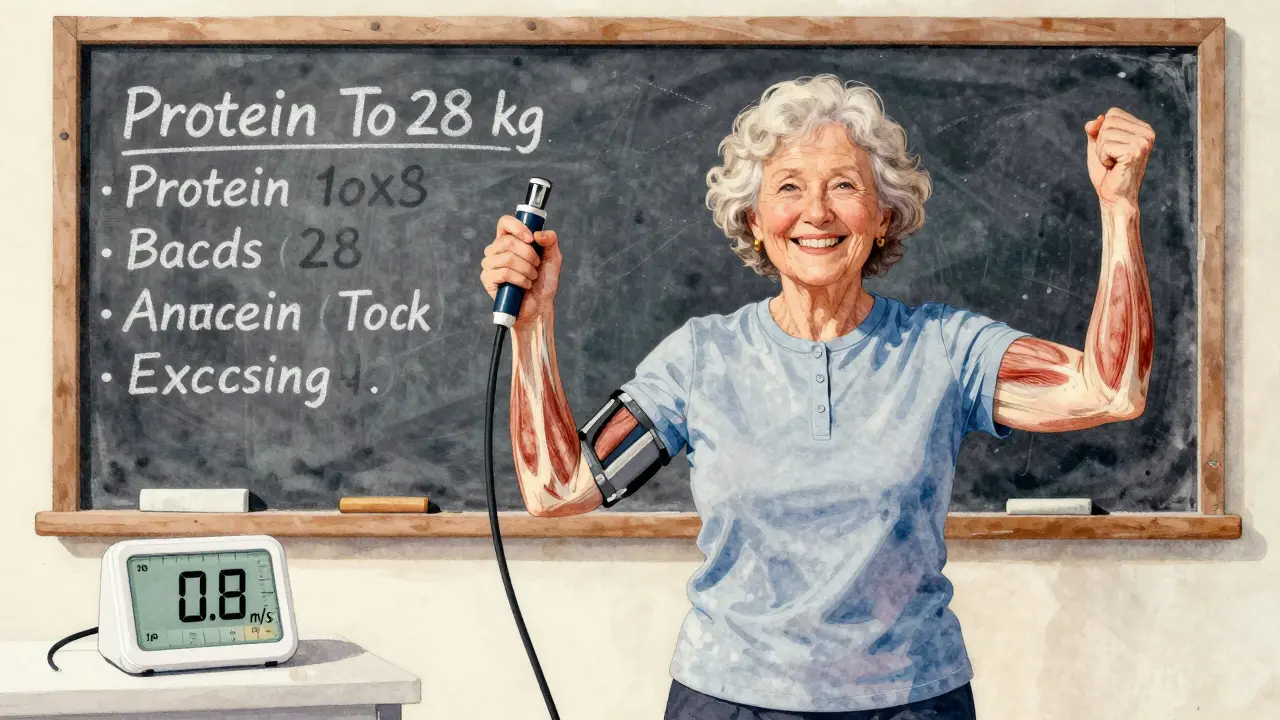
How to Know If You Have It
Doctors don’t always check for sarcopenia unless you ask. But screening is simple. The gold standard starts with a handgrip test. If you’re a man and your grip is below 27 kg (about 60 pounds), or a woman below 16 kg (35 pounds), that’s a red flag. Next, they’ll look at how fast you walk four meters. If it’s slower than 0.8 meters per second (that’s about 3 seconds to walk 10 feet), you’re at risk. For a more detailed look, a DEXA scan can measure muscle mass in your arms and legs. But even without fancy machines, you can spot signs: needing to sit down after walking across the room, struggling to lift a grocery bag, or feeling too tired to do simple chores.
There’s also a COPD-specific marker called the pectoralis muscle index (PMI). It’s measured using a chest CT scan and compares the size of your chest muscle to your body size. A PMI below 1.06 cm² per BMI unit strongly predicts sarcopenia in COPD patients. This is why BMI alone can’t be trusted-someone with COPD might have a normal weight but still be losing muscle.
What Nutrition Really Looks Like
Most people with COPD eat too little protein. The average intake? Just 0.9 grams per kilogram of body weight. But for sarcopenia, you need 1.2 to 1.5 grams per kg. That means if you weigh 70 kg (154 lbs), you need between 84 and 105 grams of protein every day. Not just at dinner. Spread across four meals. So aim for 20-25 grams per meal.
Here’s how that looks in real life:
- Breakfast: 3 eggs + 1 cup Greek yogurt = 30g protein
- Lunch: 100g chicken breast + 1 cup lentils = 40g protein
- Snack: 1 scoop whey protein shake = 25g protein
- Dinner: 150g salmon = 35g protein
That’s 130g total. Easy to overshoot? Yes. But if you’re struggling to eat enough, try protein supplements. Look for ones with added leucine-2.5 to 3 grams per serving. Leucine is the amino acid that triggers muscle building. Studies show it boosts muscle protein synthesis by 37% in sarcopenic COPD patients. Some supplements even come pre-mixed with leucine, making it easier to get the right dose.
And don’t forget calories. Many COPD patients are underweight not because they’re picky eaters, but because breathing burns so much energy. You might need 25-30 calories per kg of body weight just to maintain. So if you’re 70 kg, aim for 1,750 to 2,100 calories daily. If you’re losing weight, add healthy fats like avocado, nuts, or olive oil.
Resistance Training That Actually Works
Here’s the biggest mistake: people think they can’t lift weights because they’re out of breath. But avoiding movement makes sarcopenia worse. The key is starting slow and smart.
Begin at 30% of your one-rep max (1-RM). That’s lighter than you think. For many, that means 1- to 2-pound dumbbells or light resistance bands. Focus on big muscle groups: legs (seated leg press or chair squats), chest (seated chest press), back (seated row), and arms (bicep curls, triceps extensions). Do two sets of 10-12 reps, twice a week. Rest 2-3 minutes between sets. If you get short of breath, stop. Breathe. Then continue.
Progress slowly. After 4-6 weeks, if you’re not gasping, increase the weight by 5-10%. Most people reach 60-80% of their 1-RM within 8-12 weeks. That’s when strength gains really kick in. One study showed COPD patients improved their 6-minute walk distance by 23% after 16 weeks of this kind of training.
Important: About 42% of COPD patients need supplemental oxygen during resistance training. If you use oxygen at home, bring it with you to sessions. Many rehab centers don’t mention this upfront-and that’s why so many people quit after a few tries.
Real Stories, Real Results
Mary Thompson, 68, had GOLD Stage 3 COPD. She could barely walk to her mailbox without stopping. After joining a pulmonary rehab program, she started with resistance bands and 30 grams of protein at each meal. Twelve weeks later, she carried groceries without stopping. “I didn’t know muscle could come back,” she said.
But not everyone has a success story. John Peterson, 72, tried resistance training and had to stop after three sessions. “It made my breathing worse,” he said. “I didn’t know I needed oxygen.” His story isn’t rare. A review of 147 patient reviews found 32% quit because of breathlessness. The difference? Mary had support. John didn’t.

What Stops People From Getting Better
There are three big barriers:
- Not being screened. Only 38% of U.S. pulmonary rehab centers check for sarcopenia. If you’re not tested, you won’t be treated.
- Wrong protein intake. Most patients eat too little. Even those on supplements often don’t get enough leucine or spread their intake unevenly.
- Exercise too hard, too fast. Starting with heavy weights or no rest leads to breathlessness and quitting. Slow, steady wins the race.
Also, many people stop during flare-ups. That’s understandable-but dangerous. Muscle loss accelerates during exacerbations. Even light movement, like seated marches or arm circles, helps. Don’t wait until you feel better. Stay active, even a little.
The Future Is Here
Just last year, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) released its first-ever algorithm for managing sarcopenia in COPD. It links nighttime oxygen levels to exercise prescriptions. Early data shows a 29% drop in muscle loss for those who follow it.
Researchers are also testing new supplements like HMB (beta-hydroxy-beta-methylbutyrate), which helped preserve muscle in early trials. And a drug called PTI-501, designed to block myostatin (a protein that limits muscle growth), is in phase 2 trials for COPD patients. Results are expected in 2025.
But you don’t need to wait for drugs or trials. The tools are here now: protein, light resistance training, and oxygen support when needed. The evidence is clear. Addressing sarcopenia doesn’t just help you move better. It helps you live longer.
How do I know if I have sarcopenia with COPD?
Start with a handgrip strength test. If you’re a man and your grip is below 27 kg (60 lbs), or a woman below 16 kg (35 lbs), that’s a warning sign. Also, time yourself walking four meters. If it takes longer than 5 seconds (slower than 0.8 m/s), you may have sarcopenia. Ask your doctor about a DEXA scan or pectoralis muscle index (PMI) for a more accurate diagnosis.
How much protein do I need if I have COPD and sarcopenia?
Aim for 1.2 to 1.5 grams of protein per kilogram of body weight each day. For example, if you weigh 70 kg (154 lbs), that’s 84-105 grams daily. Spread it across 4 meals-aim for 20-25 grams per meal. Include leucine-rich sources like whey protein, eggs, chicken, or supplements with 2.5-3 grams of leucine per serving to boost muscle building.
Can I lift weights if I’m out of breath?
Yes-but start very light. Begin with 1- to 2-pound dumbbells or resistance bands. Do two sets of 10-12 reps, twice a week. Rest 2-3 minutes between sets. If you get short of breath, stop and breathe. Many people need supplemental oxygen during training-bring your oxygen with you. Slow progress is better than pushing too hard and quitting.
Why is chest muscle loss a big deal in COPD?
The pectoralis muscles help you breathe. When they weaken, your lungs can’t expand as well, making breathlessness worse. Studies show 68% of COPD patients have significant chest muscle loss, compared to only 22% of healthy people their age. This isn’t just about strength-it’s about your ability to take a full breath.
What should I do during a COPD flare-up?
Don’t stop moving completely. Even light activity helps prevent muscle loss. Try seated arm circles, ankle pumps, or marching in place while sitting. Aim for 5-10 minutes twice a day. If you’re too tired to do structured exercise, just move gently. Muscle loss accelerates during flare-ups, so even small efforts make a difference.


Ojus Save
February 13, 2026lol i read this whole thing and my only takeaway is that protein shakes are now medical equipment. also why does everyone assume i can afford 150g of salmon a day? 🤡
Rachidi Toupé GAGNON
February 14, 2026This is the kind of info that actually saves lives. 🙌 Start small - 2lb dumbbells, 3 eggs at breakfast, breathe like you mean it. You don’t need a gym. You just need to show up. 💪
Carla McKinney
February 15, 2026I’m sorry, but this article completely ignores the systemic failures in pulmonary rehab. Only 38% of centers screen? That’s not negligence - it’s institutional abandonment. And don’t get me started on how ‘light resistance training’ is coded as ‘safe’ while insurance denies home oxygen for training. This reads like a pharmaceutical ad with a side of victim-blaming.
Jim Johnson
February 15, 2026Just started this last week - 20g protein at each meal + bands. Took 3 breaks on day one. Still here. You don’t have to be strong. Just consistent. 🤘
Vamsi Krishna
February 16, 2026I’ve been doing this for 5 years and I can tell you - protein isn’t the issue. It’s the oxygen. Nobody talks about how your body is literally starving your muscles because your lungs can’t keep up. And if you don’t have a portable O2 tank, you’re just spinning your wheels. I’ve seen 3 guys quit because they were told ‘just breathe slower.’ Bro. You can’t breathe slower if your lungs are on fire.
Sophia Nelson
February 18, 2026So let me get this straight - if I’m too tired to lift a bag of rice, I’m supposed to eat more salmon and do ‘seated leg presses’? Meanwhile my Medicare copay for the dumbbells is $200. This is wellness porn for people who don’t live in a trailer with no AC.
Steve DESTIVELLE
February 19, 2026The body is a temple but also a machine that burns through fuel faster than a fighter jet. We are told to eat more protein as if it were a moral imperative. But what of the man who works two jobs and eats ramen because his breath fails him before he can afford the chicken? The solution is not individual discipline. It is structural compassion. Or we are all just dust waiting to be breathed out.
athmaja biju
February 21, 2026In India we have no access to whey protein. We have dal. We have eggs. We have coconut oil. Why are we being sold a Western solution? My aunt walks 3km every morning with a 5kg sack. She doesn’t need a DEXA scan. She needs dignity. And maybe someone to carry her groceries.
Reggie McIntyre
February 22, 2026I love how this article doesn’t mention that sarcopenia in COPD is often misdiagnosed as just ‘being old.’ My dad was told he was ‘just slowing down’ for 3 years. Then we found out his grip was 19kg and he walked slower than a snail. The PMI scan changed everything. This isn’t about fitness - it’s about survival. Don’t wait for a doctor to notice. Ask for it.
Jack Havard
February 23, 2026They say resistance training helps. But what if your oxygen tank runs out at the gym? What if your ‘rehab center’ charges $120/session and you’re on SSDI? What if the ‘leucine supplement’ is just a fancy protein powder with a 300% markup? This isn’t science. It’s capitalism with a stethoscope.
Gabriella Adams
February 25, 2026I work in pulmonary rehab. I see this every day. The people who succeed? They don’t have the best equipment. They have someone who showed up with them. A spouse. A neighbor. A grandkid. Movement is medicine. But isolation kills faster than COPD. Bring someone. Even if they just sit there. Just don’t do it alone.
Kristin Jarecki
February 25, 2026The evidence presented here is both clinically sound and deeply humane. It is imperative that healthcare systems adopt the GOLD algorithm for sarcopenia management without delay. Access to nutritional counseling and supervised resistance training must be recognized as essential components of COPD care, not optional add-ons. I urge all clinicians to prioritize screening and referral.
Jonathan Noe
February 26, 2026I’ve been doing the 20g protein per meal thing for 8 weeks. My grip went from 22kg to 31kg. I can now open a pickle jar without crying. Also - I started using my O2 during training. Game. Changer. If you’re still holding back - just try it. One session. You won’t regret it.
Brad Ralph
February 27, 2026So we’re told to eat more protein and lift light weights… while the system makes it impossible to afford oxygen, food, or time. 🤔 The real cure? A society that doesn’t treat breathing like a privilege. But hey - at least we have leucine.