18 Jan 2026
- 8 Comments
HAS-BLED Bleeding Risk Calculator
Assess Your Bleeding Risk
This tool calculates your HAS-BLED score based on key risk factors. The HAS-BLED score helps identify patients at higher risk of bleeding when taking aspirin with blood thinners.
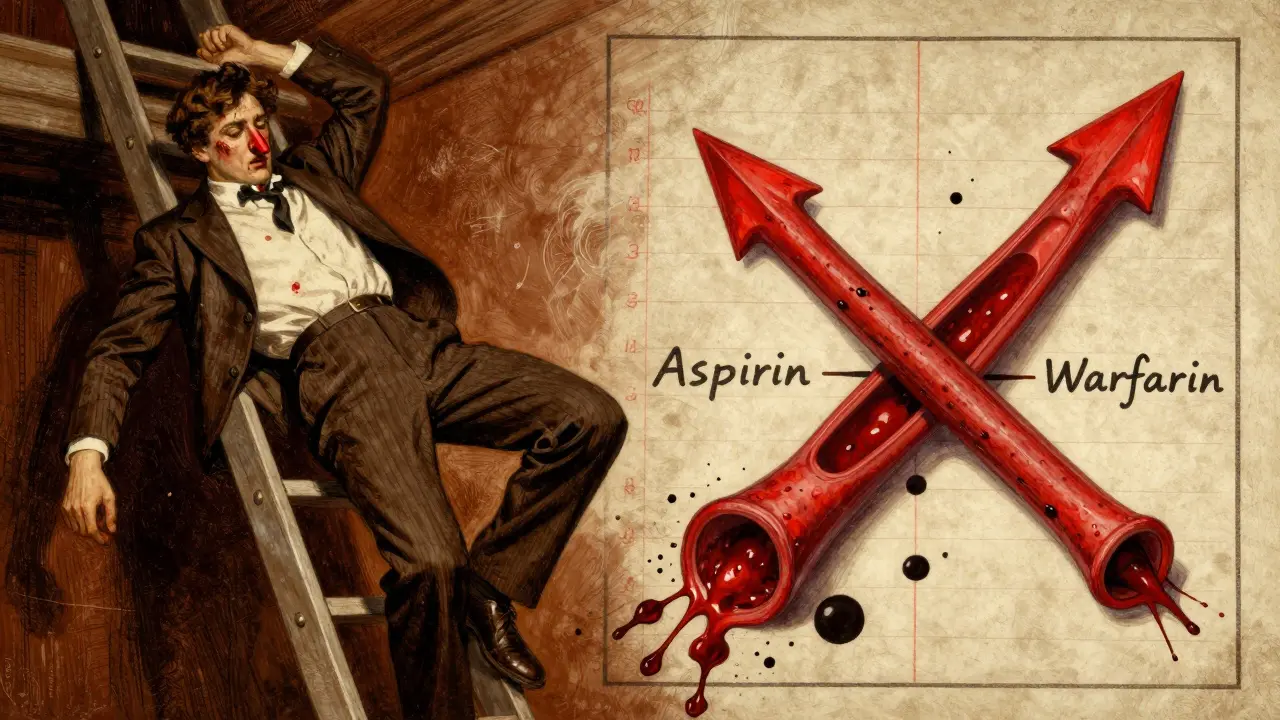
Combining aspirin with other blood thinners doesn’t just add up risks-it multiplies them. If you’re taking aspirin daily for heart health and your doctor also prescribed a blood thinner like warfarin, rivaroxaban, or apixaban, you need to understand the real danger: aspirin and blood thinners together can turn a minor cut into a life-threatening bleed.
How Aspirin and Blood Thinners Work Together-And Why That’s Dangerous
Aspirin doesn’t thin your blood the same way warfarin or Eliquis does. It works on platelets-the tiny cells in your blood that stick together to form clots. By blocking an enzyme called COX-1, aspirin stops platelets from clumping. That’s helpful if you’ve had a heart attack or stroke, because it keeps clots from forming in your arteries.
But oral anticoagulants like warfarin, Xarelto, or Pradaxa work differently. They target proteins in your blood that help the clotting process along. When you take both, you’re hitting clotting from two angles. It’s like turning off two different switches on the same machine. The result? Your blood loses its ability to seal even small injuries.
Studies show this combo doubles your chance of bleeding compared to taking just one of them. That’s not a small increase. It’s the difference between a 2% risk and a 4% risk-and when it comes to brain or stomach bleeds, even a 2% jump matters a lot.
Where the Bleeding Happens-and How Bad It Can Get
Not all bleeds are the same. Some are obvious, like a nosebleed that won’t stop. Others sneak up on you.
- Stomach and gut bleeds are the most common. People on aspirin plus a blood thinner are over twice as likely to have black, tarry stools or vomit blood.
- Brain bleeds are rarer but far more deadly. The risk goes up 3.2 times when aspirin is added to an anticoagulant. That’s why falling on your head at 70 can be far more dangerous if you’re on this combo.
- Pulmonary bleeds (in the lungs) and urinary bleeds (in the kidneys or bladder) also rise significantly.
The ASPREE trial, which followed nearly 20,000 healthy older adults, found that even low-dose aspirin (100mg daily) increased the chance of bleeding inside the skull by 38% compared to a placebo. That’s why major health groups now say healthy older people shouldn’t take aspirin just to prevent heart disease.
Not All Blood Thinners Are the Same-Here’s the Risk Ranking
If you’re on a blood thinner and your doctor suggests adding aspirin, you need to know which combo is riskiest.
Research from 2024, reviewing 24 studies, found that rivaroxaban (Xarelto) carries the highest bleeding risk when paired with aspirin. Dabigatran (Pradaxa) and apixaban (Eliquis) are slightly safer-but still risky. Warfarin, the older drug, has been studied the most. It’s tricky because its effects change based on diet, other meds, and even your genes.
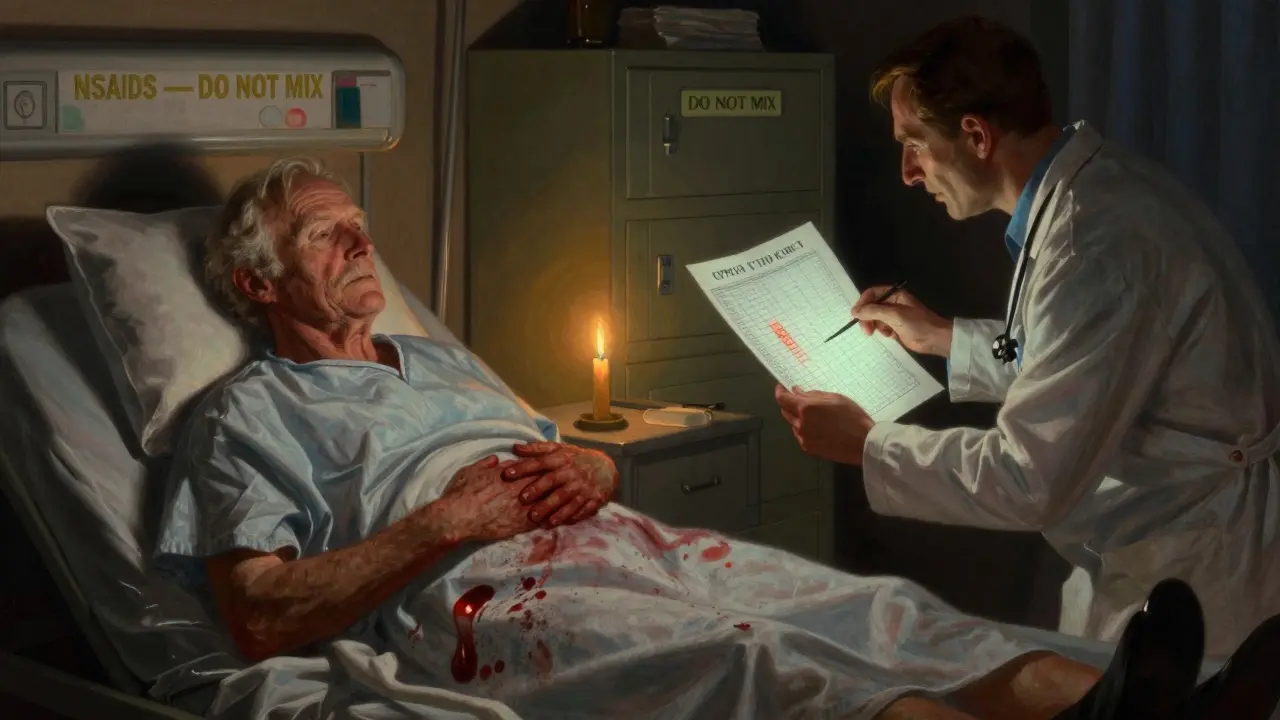
And it’s not just prescription blood thinners. Over-the-counter painkillers like naproxen (Aleve) or diclofenac (Voltaren) can be just as dangerous. Naproxen with an anticoagulant raises bleeding risk over four times. Ibuprofen (Advil) is a bit safer-but still not safe.
That’s why many doctors now avoid mixing aspirin with NSAIDs altogether. If you need pain relief, acetaminophen (Tylenol) is usually the only safe option.
Who Should Never Mix These Drugs?
Some people should avoid this combo completely:
- Anyone over 70 without a clear heart condition-routine aspirin for prevention is no longer recommended.
- People with high blood pressure, especially if it’s not well controlled.
- Those with kidney disease or a history of ulcers or GI bleeding.
- Anyone with a bleeding disorder like hemophilia or von Willebrand disease.
- People who drink alcohol regularly-alcohol irritates the stomach lining and makes bleeding more likely.
The NHS and the National Institute on Aging both agree: if you’re healthy and over 60, the risks of daily aspirin outweigh the benefits. Only take it if your doctor has a strong reason-and even then, they should check your risk score.
What to Do If You’re Already on Both
If you’re already taking aspirin and a blood thinner, don’t stop either without talking to your doctor. But do take these steps right away:
- Ask your doctor for a HAS-BLED score. It’s a simple tool that looks at your blood pressure, kidney function, age, and past bleeding history to estimate your risk.
- Get a hemoglobin blood test every 3 to 6 months. Low hemoglobin means you’re losing blood slowly-maybe from your gut.
- Use an electric razor instead of a blade. Switch to a soft-bristle toothbrush. Avoid contact sports or activities where you could fall or get hurt.
- Take aspirin with food to reduce stomach upset. Never take it on an empty stomach.
- Watch for signs: unusual bruising, blood in urine or stool, headaches that won’t go away, dizziness, or fatigue.
If you notice any of those signs, call your doctor immediately. Don’t wait.
When Is This Combo Actually Necessary?
There are a few cases where doctors still prescribe both:
- People with mechanical heart valves-these can trigger clots, so the combo is often needed.
- Some patients after stent placement, especially if they had a recent heart attack.
- Those with atrial fibrillation and a history of heart attack or blocked arteries.
In these cases, the benefit of preventing a clot (which could cause a stroke or heart attack) might outweigh the bleeding risk. But even then, doctors aim for the lowest possible aspirin dose-usually 75mg to 100mg daily-and monitor closely.
Many hospitals now use genetic tests to fine-tune warfarin dosing, especially if aspirin is involved. Genes like CYP2C9 and VKORC1 affect how your body processes the drug. If you’re on warfarin and aspirin, asking about genetic testing could help reduce your risk.
What’s Changing in 2026?
Guidelines are shifting fast. In the U.S., the number of people taking daily aspirin for prevention has dropped nearly 30% since 2019, thanks to updated advice from the U.S. Preventive Services Task Force. The global market for newer blood thinners (NOACs) is growing, but so is the number of people accidentally mixing them with aspirin.
The FDA now requires strong warning labels on NSAID packaging when sold with anticoagulants. And new research is exploring reversal agents-drugs that can quickly undo the effects of these blood thinners in an emergency.
But for now, the message is clear: unless your doctor has a solid, documented reason, don’t mix aspirin with any blood thinner. The risks are real, predictable, and often avoidable.
What to Ask Your Doctor
If you’re unsure whether you should keep taking both, ask these questions:
- Why am I on both drugs? Is there a proven benefit for my specific situation?
- What’s my bleeding risk score (HAS-BLED)?
- Could I switch to a different pain reliever instead of aspirin?
- How often should I get my blood checked?
- What are the warning signs I should never ignore?
Your doctor might not bring this up unless you ask. Don’t assume they know you’re taking aspirin-many people think it’s harmless because it’s over the counter.


Courtney Carra
January 20, 2026So let me get this straight - we’re telling people to stop taking aspirin because it might cause a bleed, but we’re fine with prescribing five other drugs that do the exact same thing? 🤔 We’ve turned medicine into a Russian roulette game where the bullet is always labeled "FDA approved."
Renee Stringer
January 22, 2026I’ve been on warfarin for 8 years. My doctor added aspirin because I had a stent. I didn’t question it until I started bleeding out of my gums every morning. Now I’m on 81mg aspirin only on days I feel chest pressure. No more daily. I’m not a statistic.
kumar kc
January 22, 2026Aspirin + blood thinner = bad. Stop mixing. End of story.
Jacob Cathro
January 23, 2026ok but like… the real issue here is that doctors are still prescribing this like it’s 2005. NSAIDs? Bro. I took ibuprofen with Eliquis for a week and my stool looked like a chocolate milkshake. I didn’t go to the doc till I passed out in Target. Now I use tylenol and a heating pad. And yes, I still take my meds. But I’m not your lab rat.
Edith Brederode
January 24, 2026This is exactly why I always ask my pharmacist before taking anything new. I don’t trust doctors to read the full label. I’ve had two friends die from GI bleeds from this combo. Please, if you’re on both - get a second opinion. Seriously.
Arlene Mathison
January 25, 2026Listen. I’m 68. Healthy. No heart issues. Took aspirin for "prevention" because my cousin said it was a miracle. Turns out, I had a silent ulcer. Bleeding for months. Hemoglobin dropped to 7. I didn’t know until I passed out in the grocery store. Don’t be like me. Ask questions. Get tested. Your body isn’t a spreadsheet.
thomas wall
January 25, 2026The medical establishment’s failure to adequately communicate the cumulative risk of polypharmacy is not merely a clinical oversight - it is an ethical failure of monumental proportion. The normalization of aspirin as a benign prophylactic, despite overwhelming evidence of its pro-hemorrhagic synergy with anticoagulants, reflects a systemic devaluation of patient autonomy and a pathological reliance on protocol over personalized risk assessment. We are not treating patients; we are managing populations. And the cost? Lives reduced to p-values.
Emily Leigh
January 25, 2026Wait… so if I’m on apixaban and I take one aspirin for a headache… I’m basically playing Russian roulette with my brain? 😳 And nobody told me? I’ve been doing this for 3 years. I’m going to call my doctor right now. Also - why is Tylenol the only safe option? Because it’s cheaper? Or because Big Pharma doesn’t make enough profit off it? 🤔