23 Oct 2025
- 10 Comments
Allopurinol Dose Calculator
Allopurinol Dosing Assistant
This tool calculates appropriate starting doses for Allopurinol based on kidney function (eGFR) as recommended by rheumatology guidelines.
Recommended Starting Dose
Important Safety Information
When dealing with Gout is a form of inflammatory arthritis caused by high uric acid levels, many doctors prescribe Allopurinol as the cornerstone medication. This guide walks you through the science, the dosing tricks, and the day‑to‑day habits that keep flare‑ups at bay.
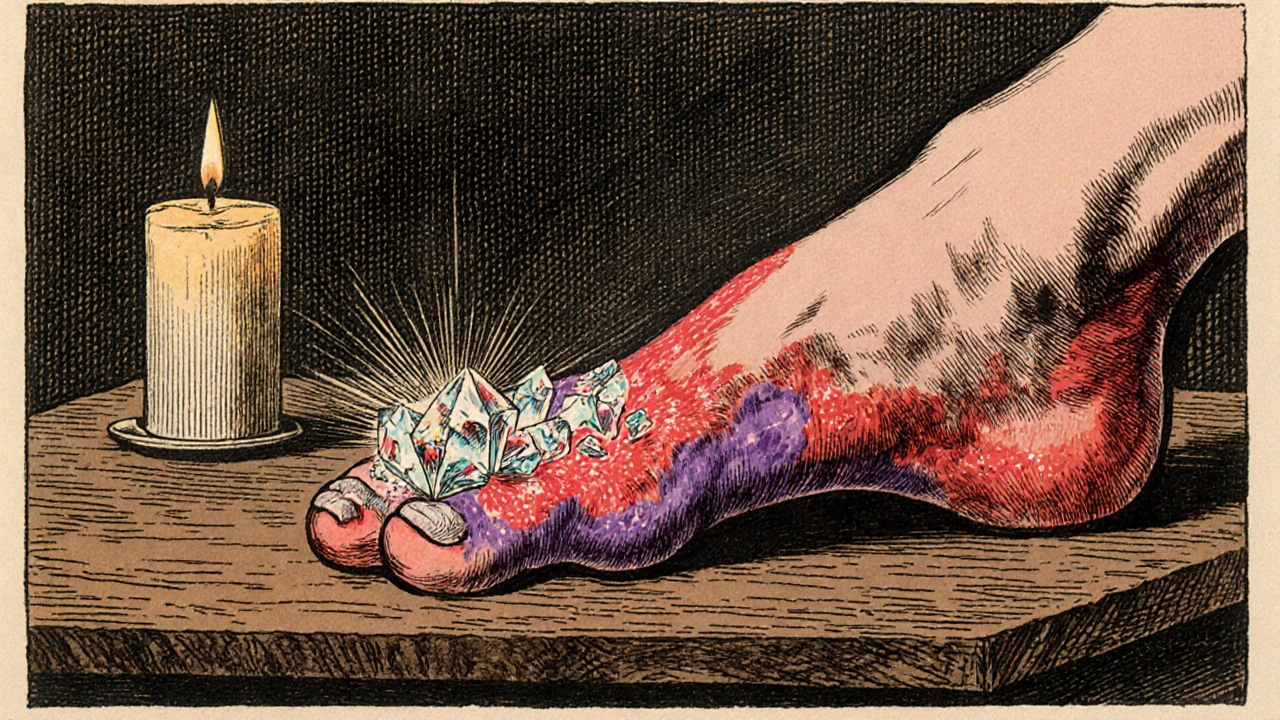
What Is Gout and Why Does It Flare?
Gout occurs when uric acid crystals accumulate in joints, most often the big toe. The crystals trigger an intense immune response, causing the classic burning pain, swelling, and redness. A single episode can last days, but repeated attacks damage cartilage and lead to chronic arthritis.
Three key drivers push uric acid over the limit:
- Overproduction of uric acid, often due to genetics or high‑purine foods.
- Under‑excretion by the kidneys, a condition called Hyperuricemia.
- Secondary factors like alcohol, certain diuretics, and metabolic syndrome.
Understanding these triggers helps you pair medication with lifestyle tweaks for lasting control.
How Allopurinol Works
Allopurinol is a Xanthine Oxidase inhibitor. By blocking this enzyme, it reduces the conversion of purines into uric acid, gradually lowering blood levels. Unlike painkillers that treat a flare after it starts, Allopurinol acts preventively, keeping the uric‑acid “tank” from filling up.
Because the drug works on production, you won’t feel immediate relief when a flare begins. That’s why doctors often combine Allopurinol with fast‑acting agents such as NSAIDs or Colchicine during acute attacks.
Setting Up an Allopurinol Regimen
Starting Allopurinol is a balancing act. Too low a dose won’t curb uric acid; too high can cause rash or, in rare cases, severe hypersensitivity. Here’s a step‑by‑step approach most rheumatologists follow:
- Baseline labs: serum uric acid, kidney function (eGFR), liver enzymes.
- Initial dose: 100 mg daily for most adults; 50 mg for those with eGFR < 30 mL/min.
- Increase by 100 mg every 2-4 weeks, aiming for a target uric acid ≤ 6 mg/dL (≤ 5 mg/dL if tophi are present).
- Monitor labs after each dose change, especially for allergic skin reactions.
- Maintain the final dose for at least 6 months before considering taper.
Take the tablet with food to minimise stomach upset, and stay consistent-missing doses can cause uric‑acid rebound.
Managing a Flare While on Allopurinol
Even with optimal dosing, a flare can sneak in, often triggered by diet or dehydration. When that happens, follow these rapid‑action steps:
- Rest the joint. Elevate and apply an ice pack for 20 minutes, several times a day.
- Start an NSAID. Ibuprofen 400 mg every 6 hours (if kidneys are healthy) or naproxen 250 mg twice daily.
- Consider colchicine. A loading dose of 1.2 mg, then 0.6 mg one hour later, works well for early attacks.
- Hydrate. Aim for at least 2.5 L of water daily; urine dilution helps flush uric acid.
- Avoid alcohol and high‑purine meals. Red wine and organ meats can reignite crystal formation.
If pain persists beyond 48 hours, contact your clinician. Sometimes a short corticosteroid burst is needed.
Lifestyle Strategies to Boost Allopurinol Effectiveness
Medication is only half the battle. Pairing Allopurinol with the right habits can slash flare‑up frequency by up to 70 %.
- Purine‑smart diet. Limit seafood (anchovies, sardines), red meat, and sugary drinks. Embrace low‑purine foods like dairy, cherries, and whole grains.
- Weight management. Each kilogram of excess weight adds roughly 0.5 mg/dL to serum uric acid. Gradual loss of 5-10 % body weight improves control.
- Consistent hydration. Aim for urine that is light straw‑colored; dark urine signals dehydration.
- Alcohol moderation. Beer is especially problematic because it contains guanosine, a purine precursor.
- Review medication list. Diuretics (e.g., hydrochlorothiazide) and low‑dose aspirin can raise uric acid; discuss alternatives with your doctor.
Common Pitfalls and How to Avoid Them
Even seasoned patients trip up. Spot the red flags early:
- Skipping the titration phase. Jumping straight to 300 mg can spike rash risk.
- Ignoring kidney function. Doses above 300 mg in patients with eGFR < 50 mL/min increase toxicity.
- Stopping Allopurinol during a flare. The drug needs to stay on board; otherwise uric‑acid levels rebound.
- Taking vitamin C megadoses. While modest doses (≤ 500 mg) may lower uric acid, high doses can interact with Allopurinol and cause kidney stones.
Set reminders, keep a medication log, and schedule lab checks every 3-6 months.
Allopurinol vs. Other Gout‑Lowering Drugs
| Attribute | Allopurinol | Febuxostat | Probenecid |
|---|---|---|---|
| Mechanism | Xanthine Oxidase inhibitor | Selective Xanthine Oxidase inhibitor | Urate reabsorption blocker |
| Typical dose | 100-300 mg daily | 40-80 mg daily | 500-2000 mg daily (divided) |
| Kidney safety | Requires dose reduction if eGFR < 30 | Can be used down to eGFR = 30 | Contraindicated in severe renal impairment |
| Cardiovascular risk | Neutral | Potential increased risk in high‑risk patients | Neutral |
| Common side‑effects | Rash, GI upset, rare hypersensitivity | Elevated liver enzymes | Kidney stones, GI upset |
If you have chronic kidney disease, Allopurinol often remains the first line, but Febuxostat is a solid backup when doses need to stay low. Probenecid works best for younger patients who over‑excrete uric acid and have good kidney function.
Quick Checklist for Daily Success
- Take Allopurinol at the same time each day with food.
- Drink at least 2.5 L of water.
- Limit purine‑rich foods to < 3 servings per week.
- Avoid beer and excess liquor.
- Schedule lab check every 6 months.
- Keep a flare‑log: triggers, meds taken, outcome.
Frequently Asked Questions
Can I start Allopurinol during an active gout flare?
It’s generally not recommended because the drug can shift uric‑acid levels and worsen the flare. Begin a tapering schedule when the flare subsides, using NSAIDs or colchicine for immediate relief.
How long does it take to see a drop in uric‑acid levels?
Most patients see a measurable reduction within 2-4 weeks of a stable dose, but full therapeutic effect often needs 3-6 months.
Is a rash a sign I should stop Allopurinol?
Yes. A widespread or blistering rash could indicate hypersensitivity, a rare but serious reaction. Contact your doctor immediately; they may switch you to febuxostat.
Can I take vitamin C with Allopurinol?
Low‑dose vitamin C (≤ 500 mg) is usually safe and may modestly lower uric acid. High doses increase the risk of kidney stones, so keep supplementation modest.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one and resume your regular schedule. Do not double‑dose.
By weaving together proper dosing, quick‑action flare care, and everyday lifestyle tweaks, you can keep the painful attacks of gout well under control. Remember, Allopurinol is a long‑term ally-not a rescue pill-so consistency is the name of the game.

Shan Reddy
October 23, 2025Thanks for the clear guide – I’ll definitely keep a daily water log.
CASEY PERRY
October 24, 2025The titration schedule aligns with pharmacokinetic principles, ensuring steady-state plasma concentration without precipitating hypersensitivity.
Naomi Shimberg
October 26, 2025Despite the prevailing consensus, the purported benefit of low‑dose vitamin C in urate reduction remains statistically insignificant, thereby rendering routine supplementation an unnecessary adjunct to allopurinol therapy.
Heather ehlschide
October 27, 2025Allopurinol dosing should always begin after an acute flare has resolved to avoid exacerbating purine turnover.
Baseline renal function determines the initial dose, with eGFR below 30 mandating a 50 mg start.
Incremental titration by 100 mg every 2–4 weeks allows the body to adapt and minimizes rash risk.
Serum uric acid should be rechecked 4 weeks after each dose adjustment.
The therapeutic target of ≤6 mg/dL reduces crystal formation and long‑term joint damage.
If tophi are present, aiming for ≤5 mg/dL yields better resolution of deposits.
Consistency is key; missing doses creates a rebound surge in uric acid levels.
Hydration of at least 2.5 L daily dilutes urine and aids renal excretion of urate.
Dietary purine restriction complements pharmacotherapy, especially limiting red meat and certain seafood.
Alcohol, particularly beer, should be limited because it provides guanosine, a purine precursor.
Monitoring for rash or fever is crucial, as hypersensitivity can be life‑threatening.
Should a rash appear, discontinue immediately and consider febuxostat as an alternative.
NSAIDs or colchicine can be employed for breakthrough flares while allopurinol maintains baseline control.
Chronic kidney disease patients often tolerate reduced allopurinol doses better than febuxostat.
Maintaining a simple medication log and lab schedule every 6 months streamlines long‑term management.
Kajal Gupta
October 28, 2025Yo, this guide is like a recipe for kicking gout to the curb – splash some water, ditch the beer, and let the cherry juice work its magic. Trust me, the toe will thank you!
Zachary Blackwell
October 29, 2025Honestly, the whole “follow the doctor’s titration plan” narrative feels like a profit‑driven script pushed by pharma giants to keep us buying brand‑name pills forever.
Michaela Dixon
October 30, 2025I get where you’re coming from the idea that big pharma pulls the strings but think about how many lives have actually improved with allopurinol it’s not all smoke and mirrors the drug has decades of data supporting its safety when used correctly you just have to stay vigilant about kidney function and rash warnings and yes the dosing schedule can seem like a money‑making scheme but at the end of the day it’s about balance between efficacy and safety so maybe the answer lies in personalized medicine not blanket conspiracy theories
Dan Danuts
October 31, 2025Great summary! Keep that water bottle handy and you’ll crush those flares.
keerthi yeligay
November 1, 2025Stay consistent with the dose and hydrate – small steps lead to big results.
kenny lastimosa
November 3, 2025In the grand scheme, managing uric acid is a reminder that even the smallest chemical imbalances can ripple into profound pain, urging us to respect the delicate equilibrium of the body.