5 Jan 2026
- 11 Comments
Thyroid Eye Disease (TED) isn’t just about dry eyes or puffy eyelids. It’s an autoimmune condition where your body’s immune system attacks the tissues behind your eyes-muscles, fat, connective tissue-and turns them into inflamed, swollen messes. It’s linked to Graves’ disease, but you don’t need to have an overactive thyroid to get it. Some people develop TED with normal thyroid levels. Others get it after their thyroid has been treated-or even removed. And if you’re a woman over 40 who smokes? Your risk jumps dramatically.
What Does Thyroid Eye Disease Actually Feel Like?
People often dismiss early signs as allergies or tiredness. But TED doesn’t go away with rest. A gritty, sandy feeling in the eyes? That’s common-78% of patients report it. Light sensitivity? That’s not just bright sun; it’s pain from inflamed tissues. About half say their eyes hurt when they move them. Redness? Not just from rubbing. It’s swelling of the conjunctiva, the clear layer over the white of the eye. Dry eyes? Yes, but also excessive tearing-your eyes are trying to wash out the irritation.
Then there’s the bulging. Proptosis-eyes pushed forward-isn’t rare. One in three people with moderate-to-severe TED have it badly enough to be noticeable. Double vision? That happens when the eye muscles swell and stick together, preventing smooth movement. You might catch yourself tilting your head just to see straight. And it’s almost always both eyes. Only 11% of cases are one-sided.
Doctors use something called the Clinical Activity Score (CAS) to measure how active the disease is. If your score hits 3 or higher, you’re in the inflammatory phase. That’s when treatment needs to start fast-before the tissue hardens into permanent scar tissue. Once that happens, no drug can undo it. Only surgery can help.
Why Steroids Are Still the First Line-but Not the Whole Story
For years, steroids have been the go-to for active TED. They quiet the immune system. Intravenous methylprednisolone is the gold standard: 500 mg once a week for six weeks, then 250 mg for another six. About 60-70% of people see real improvement in swelling, redness, and double vision. It works faster than oral steroids, and the side effects are less severe-though still real.
Oral prednisone? It’s cheaper and easier, but you pay for it later. Up to 30% of people relapse after stopping. And the side effects? Weight gain-on average 8.2 kg. Blood sugar spikes. Bone thinning. Mood swings. One patient on Reddit said, “I gained 30 pounds and got prediabetes in six weeks.” That’s not just inconvenient-it’s dangerous.
Guidelines now say to cap IV steroid doses at 4.5-5.0 grams total. Go over that, and liver damage becomes a real risk. That’s why many doctors now look for alternatives before pushing patients through a full steroid course.
The Game Changer: Biologics and Teprotumumab
In 2020, the FDA approved teprotumumab (Tepezza®), and everything changed. For the first time, there was a drug that didn’t just suppress inflammation-it targeted the root cause.
Teprotumumab blocks the IGF-1 receptor, which is overactive in TED tissue. In the OPTIC trial, 71% of patients saw their eyes bulge back by at least 2 millimeters. That’s not subtle. That’s life-changing. Double vision improved in 59% of patients, compared to just 26% on placebo. And the improvements lasted.
The treatment? Eight infusions, every three weeks. Each one takes about an hour. You sit, you get hooked up, you watch a show. No hospital stay. No daily pills.
But it’s expensive. In the U.S., one full course costs around $360,000. Insurance fights it. One patient said, “The $5,000 per infusion nearly bankrupted me-even with insurance.” Medicaid patients face denials 67% of the time. Commercial insurance? Still 42% get denied. The average wait for approval? 47 days. That delay can mean the difference between saving vision and needing surgery.
Side effects? Muscle spasms in 24%. Hearing changes in 11%. High blood sugar in 8%. The FDA added a boxed warning for these. But compared to steroids? Far fewer systemic effects. Patient satisfaction? 74% for biologics vs. 58% for steroids.

What About Other Biologics?
Teprotumumab isn’t the only option on the horizon. Satralizumab (Enspryng®), approved in 2023, is a subcutaneous injection that blocks IL-6, another key player in inflammation. It’s easier to take at home and costs less than teprotumumab. Early data shows a 54% response rate for proptosis reduction.
Rituximab and tocilizumab have been tried too, but results are mixed. They’re not FDA-approved for TED, so they’re used off-label-and insurance rarely covers them. The evidence isn’t strong enough yet to make them first choices.
And now? Amgen, which bought Horizon Therapeutics (the maker of Tepezza), is developing a biosimilar. Expected by 2025, it could cut costs by 30-40%. That’s huge for access.
What You Can Do Right Now
If you’ve been diagnosed with TED-or think you might have it-here’s what matters most:
- Stop smoking. It increases your risk of severe TED by nearly eight times. Quitting won’t reverse damage, but it stops it from getting worse.
- Get your TRAb levels tested. If they’re above 15 IU/L, your risk of TED is nearly five times higher. Knowing this early lets your team act before symptoms start.
- Use preservative-free artificial tears. For mild cases, sodium hyaluronate drops help 85% of people within four weeks. Simple. Safe. Effective.
- Consider selenium. A daily 200 mcg supplement showed modest improvement in quality of life for mild TED. Not a cure, but it’s low-risk and backed by a Cochrane review.
- Get imaging. CT or MRI scans show which eye muscles are swollen. The inferior and medial rectus are most often affected. That helps predict what kind of double vision you’ll get-and whether surgery might be needed later.
When Surgery Comes In
Surgery isn’t the first step. It’s the last. You wait until the disease is inactive-usually after 6-24 months of inflammation. If you jump in too early, swelling changes after surgery, and you end up with worse alignment.
Orbital decompression removes bone to create space for swollen tissues. It reduces bulging by 2-5 mm. But 15% of patients get new or worse double vision. Sinus infections happen in 8%. Vision loss? Rare-0.5%-but real.
Strabismus surgery fixes misaligned eyes. Prisms in glasses help 60% of people with mild double vision. But if the muscle imbalance is over 15 prism diopters? Prisms won’t cut it. Surgery becomes the only option.
Reconstructive surgery for eyelids? That’s for when the lids can’t close properly, risking corneal damage. It’s often done after decompression.
The Big Picture: Access, Equity, and the Future
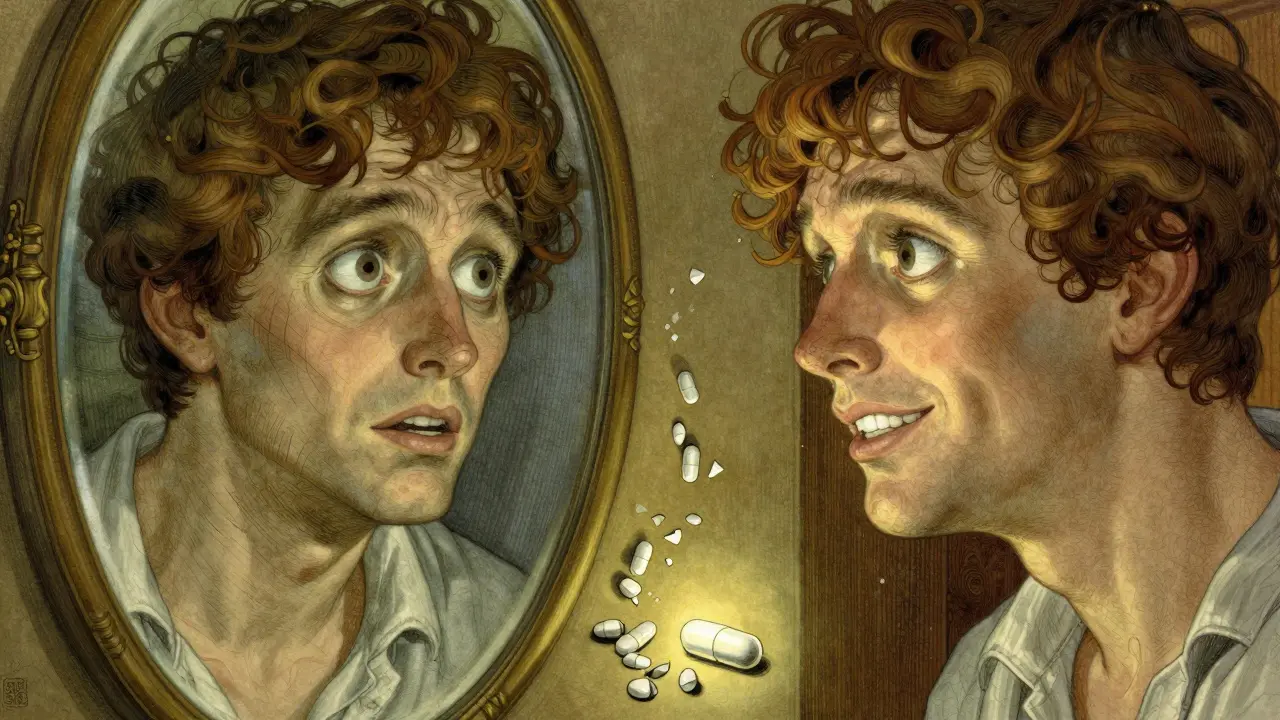
TED is rare-16 cases per 100,000 people a year. But its impact is huge. People lose jobs. They can’t drive. They avoid mirrors. Depression rates are high.
Access is the biggest barrier. Only 45% of U.S. ophthalmologists routinely use biologics. In rural areas? Just 28% have access to specialized TED centers. Insurance battles delay care. Patients wait months. By then, the window for medical treatment closes.
Research is moving fast. The TOPAZ trial is testing teprotumumab plus selenium. Early results show an 82% response rate-better than either alone. Genetic studies are looking for biomarkers that predict who’ll respond to what. One expert predicts personalized therapy within five years.
For now, the message is clear: if you have TED, don’t wait. Get tested. Get treated early. Steroids still work-but biologics offer a better path. And if you’re denied coverage? Fight it. Document everything. Ask for peer-to-peer review. There are patient advocacy groups that help.
Thyroid Eye Disease isn’t just an eye problem. It’s a whole-body autoimmune condition that needs expert care. And the tools to treat it-really treat it-are finally here. The question isn’t whether you can afford treatment. It’s whether you can afford not to try.
Can you get Thyroid Eye Disease without having Graves’ disease?
Yes. While most cases occur in people with Graves’ disease, about 10-15% of TED patients have normal thyroid function (euthyroid) or even an underactive thyroid (hypothyroidism). The autoimmune process targets the same tissues behind the eyes regardless of thyroid hormone levels.
How quickly do steroids work for Thyroid Eye Disease?
Intravenous steroids often show improvement in redness, swelling, and double vision within 2-4 weeks. Some patients notice reduced eye pain and better eye movement after just one or two infusions. But full results usually take 8-12 weeks. Starting early-within two weeks of symptom onset-boosts success rates from 42% to 65%.
Is teprotumumab (Tepezza) worth the cost?
For many, yes. Clinical trials show 71% of patients had significant reduction in eye bulging, and nearly 60% saw double vision improve. Compared to steroids, it has fewer long-term side effects like weight gain and diabetes. While the $360,000 price tag is steep, many patients say the improvement in vision, appearance, and quality of life makes it worth fighting for insurance coverage. Biosimilars expected by 2025 may lower costs significantly.
Can thyroid eye disease cause permanent vision loss?
Yes, but it’s rare. The main risk comes from optic neuropathy-when swollen muscles crush the optic nerve. This happens in about 5% of severe cases and can lead to permanent vision loss if not treated immediately. Symptoms include sudden vision dimming, color fading, or loss of peripheral vision. This is a medical emergency requiring urgent steroid treatment or surgery.
Does smoking make thyroid eye disease worse?
Absolutely. Smoking increases your risk of developing TED by 7.7 times and makes it 3-5 times more likely to become severe. It also reduces the effectiveness of both steroids and biologics. Quitting at any stage helps slow progression and improves treatment outcomes. Even if you’ve had TED for years, quitting still matters.
Are there any natural remedies that help with TED?
Selenium supplementation (200 mcg daily) is the only natural option with solid evidence. A Cochrane review found it modestly improves quality of life in mild TED, especially in early stages. Other supplements like omega-3s or antioxidants have no proven benefit. Avoid high-dose iodine-it can trigger or worsen thyroid autoimmunity. Always talk to your doctor before starting anything.
What should I do if my insurance denies teprotumumab?
Don’t accept the denial as final. Request a peer-to-peer review with your doctor and the insurer’s medical director. Submit clinical documentation showing your CAS score is ≥3 and that steroids failed or weren’t tolerated. Many patients succeed on appeal. Patient advocacy groups like the Graves’ Disease & Thyroid Foundation offer free help with appeals and financial assistance programs.
Next Steps for Patients
If you’re newly diagnosed:
- Get a full thyroid panel and TRAb test.
- See an ophthalmologist who specializes in TED-not just any eye doctor.
- Start preservative-free artificial tears and quit smoking today.
- Ask about your Clinical Activity Score. If it’s 3 or higher, push for treatment within two weeks.
- Research your insurance coverage for teprotumumab. Call your insurer and ask: “Is Tepezza covered under my plan? What’s the prior authorization process?”
If you’re already on steroids and side effects are unbearable, talk to your doctor about switching to biologics. If you’ve had surgery but still have double vision or dry eyes, ask about prisms or specialized lubricants. TED is complex, but it’s not hopeless. With the right team and timing, most people regain their vision-and their confidence.


Ashley S
January 6, 2026So basically if you're a woman who smokes and has thyroid issues, you're basically signing up for a horror movie? 🤦♀️ I knew my dry eyes were bad, but I didn't think I was one step away from looking like a alien. I'm just glad I quit smoking last year-still scared to look in the mirror though.
Beth Templeton
January 7, 2026Selenium? Really? That's your big hope? You're telling me we're still treating autoimmune eye damage with a mineral supplement like it's 2005?
Katie Schoen
January 8, 2026Okay but imagine paying $360k for a drug that makes your muscles spasm and your ears ring… and then your insurance says no. 😭 I had a friend go through this. She cried in the parking lot after her 3rd denial. She’s now on a GoFundMe. This isn’t healthcare. It’s a capitalist nightmare.
Kelly Beck
January 8, 2026You are NOT alone. Seriously. I was diagnosed with TED last year and thought I was doomed. I was terrified to leave the house. But after 8 infusions of Tepezza? I can see my own eyes in the mirror again without crying. I know it’s expensive, but if you can fight for it-please do. There are patient advocates who will literally walk you through the appeals process. You’ve got this. 💪❤️
Molly McLane
January 10, 2026One thing people don’t talk about enough: the emotional toll. It’s not just the bulging eyes or double vision-it’s the way people stare. Or don’t look at you at all. I stopped going to family gatherings because I felt like a spectacle. Tepezza didn’t just fix my eyes-it gave me back my dignity. If you’re considering it, don’t wait. The window is real. And yes, smoking is the enemy. I quit cold turkey after my diagnosis. Best decision I ever made.
Mukesh Pareek
January 10, 2026The entire paradigm of TED management remains fundamentally flawed. Steroids are merely immunosuppressive band-aids, whereas teprotumumab’s IGF-1R antagonism represents a paradigmatic shift toward targeted immunomodulation. The pharmacoeconomic arguments against it are myopic-when you factor in long-term surgical costs, lost productivity, and psychiatric comorbidities, the cost-benefit ratio becomes overwhelmingly favorable. We’re not discussing a luxury drug; we’re discussing a disease-modifying intervention.
Indra Triawan
January 12, 2026I read this whole thing and I just feel… empty. Like all this science and money and fighting, and still no one talks about how it feels to wake up and your eyes are just… not yours anymore. Like someone else’s face got glued to your skull. I don’t need stats. I need someone to say: I see you. And you’re not broken.
Isaac Jules
January 14, 2026Oh please. Tepezza is just a fancy placebo with a $360k price tag. I’ve seen 3 patients on it-two got worse. The ‘improvement’ is mostly just temporary swelling reduction. And don’t get me started on the muscle spasms-those aren’t side effects, they’re the drug screaming at you. This is pharma exploiting desperate people. Don’t be fooled.
Tiffany Adjei - Opong
January 15, 2026Wait-so if I’m a 45-year-old woman who never smoked and has normal thyroid levels, I’m still at risk? So… what’s the point of even trying to be healthy? 😏 I mean, if my body’s just gonna turn on me anyway, why bother eating kale or sleeping 8 hours? At least I can enjoy my cigarette while I still can.
Lily Lilyy
January 15, 2026To anyone reading this who feels hopeless: You are not alone. You are worthy. You are not your eyes. I was told I’d never drive again. Now I drive my kids to school every day. It took time. It took fighting. It took believing in myself when no one else did. Please, reach out. There are people who will hold your hand through this. You are loved. 🌻
Matt Beck
January 16, 2026So… I got Tepezza approved after 3 appeals. 8 infusions. Muscle spasms? Yeah. But I can see my own reflection again. And I didn’t need surgery. I cried in the infusion chair. Not from pain. From relief. 🥹 I’m not a hero. I just didn’t give up. If you’re reading this… don’t give up either. 💙