18 Nov 2025
- 13 Comments
Hypertensive Crisis Drug Interaction Checker
Check Your Medications
Enter your current medications to see if they interact dangerously with blood pressure. The tool highlights common combinations that can cause hypertensive crisis.
Potential Danger!
These combinations can cause severe hypertensive crisis (BP > 180/120 mmHg).
- Go to the emergency room immediately
- Do not take any additional medications
- If you have an MAOI, avoid tyramine-containing foods
No Dangerous Interactions Found
These medications do not have dangerous interactions for hypertensive crisis according to current knowledge.
- Continue monitoring your blood pressure
- Check with your doctor about any concerns
- Be aware of common triggers like black licorice
A severe hypertensive crisis isn’t just a bad headache or a spike on your home monitor. It’s a medical emergency where your blood pressure rockets past 180/120 mmHg-sometimes over 220/130-and your organs start shutting down. Blood vessels burst, kidneys fail, the brain swells, and the heart struggles to pump. And shockingly, drug interactions are behind nearly one in five of these life-threatening events.
Most people think high blood pressure is about salt, stress, or being overweight. But what if it’s your medication? Or worse-what if it’s your medication mixing with something else? A common cold pill. A piece of aged cheese. A new antidepressant. These aren’t rare edge cases. They’re happening every day in emergency rooms across the UK and beyond.
How a Simple Drug Mix Can Trigger a Crisis
It starts with a simple interaction. One drug blocks a natural brake in your body. Another one slams the gas pedal. The result? Your blood pressure doesn’t just rise-it explodes.
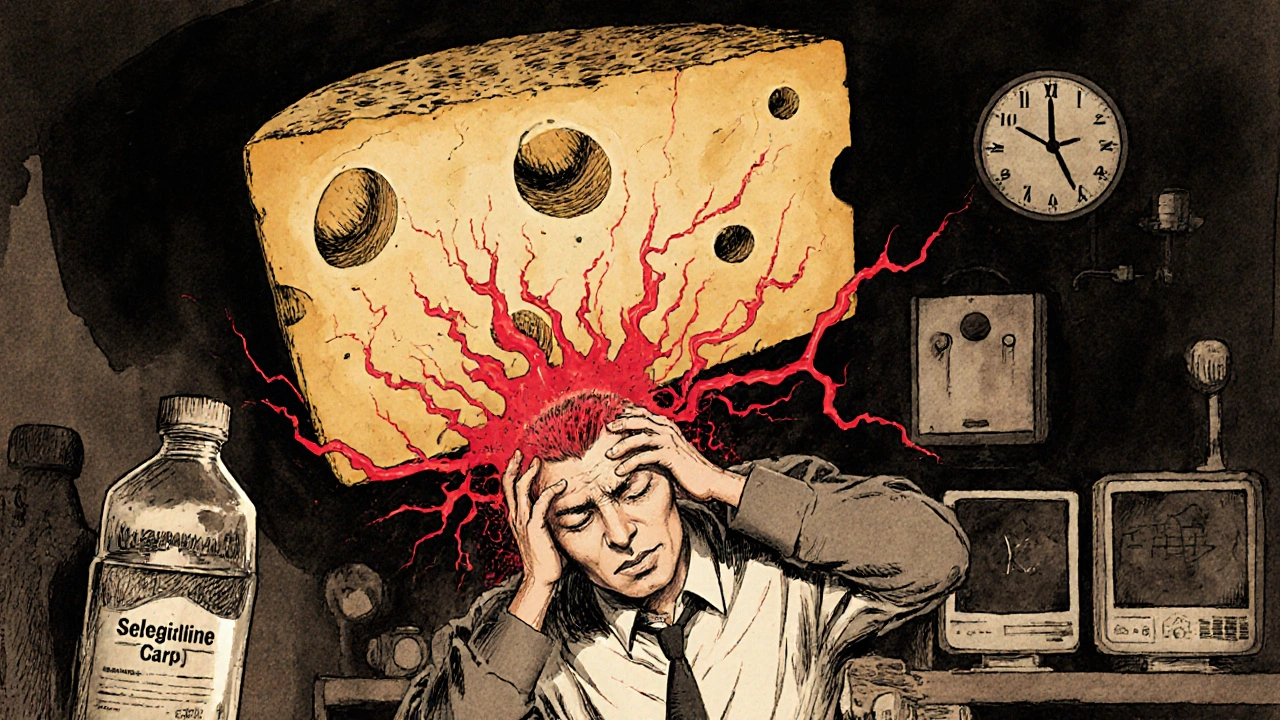
Take MAOIs, a class of older antidepressants like phenelzine or selegiline. They stop your body from breaking down tyramine, a compound found in aged cheese, cured meats, and fermented foods. Normally, your body handles tyramine fine. But with an MAOI in your system, tyramine floods your bloodstream, forcing massive amounts of norepinephrine into your blood vessels. Within minutes, your systolic pressure can jump 50 to 100 mmHg. Cases have been documented where patients hit 250 mmHg after eating a slice of cheddar. One Reddit user described waking up with 220/130 after cheese and selegiline-three days in ICU, still terrified of dairy.
Then there’s cocaine. It’s not just illegal-it’s a ticking time bomb when mixed with beta-blockers like propranolol. Cocaine causes blood vessels to constrict. Propranolol blocks the heart’s beta receptors but leaves the alpha receptors wide open. Without the beta brake, the alpha constriction goes unchecked. Systolic pressures over 220 mmHg have been recorded within an hour of taking both. This isn’t theoretical. It’s in the medical literature. And it’s fatal if not treated immediately.
The Hidden Culprits You’re Not Thinking About
It’s not just street drugs or old antidepressants. The most dangerous interactions often come from things you’d never suspect.
Think about venlafaxine, a widely prescribed SNRI antidepressant. At doses under 150 mg/day, it’s generally safe. But above 300 mg/day, it starts pushing diastolic pressure above 90 mmHg. That’s not a fluke. A 2015 meta-analysis confirmed this dose-dependent effect. And here’s the kicker: many doctors don’t check blood pressure after increasing the dose. Patients report headaches, dizziness, blurred vision-and are told it’s “just anxiety.”
Even more surprising? Over-the-counter decongestants. Pseudoephedrine, found in cold and allergy pills, is a powerful stimulant. It’s fine for a healthy person. But if you’re on an antidepressant, a beta-blocker, or even have untreated hypertension, it can trigger a crisis. Consumer Reports found only 12% of these products carry clear warnings about blood pressure risks.
Then there’s licorice. Yes, candy. Black licorice contains glycyrrhizin, which blocks the enzyme that protects your body from cortisol acting like a mineralocorticoid. That means your body starts retaining sodium like a sponge-blood volume swells by 10-15%, potassium drops, and your pressure climbs. One patient in the UK traced his persistent hypertension to daily licorice sweets. After quitting, his BP returned to normal in two weeks.
Cyclosporine, used after organ transplants, affects up to half of patients. It causes blood vessels to tighten and kidneys to hold onto sodium. But doctors often mistake the rising pressure for organ rejection-and give more immunosuppressants. That makes it worse.
Why This Is So Often Missed
Here’s the uncomfortable truth: doctors don’t ask the right questions.
A 2021 survey found 68% of patients who suffered a drug-induced hypertensive crisis had already reported symptoms like headaches or vision changes-but only 22% had their meds reviewed. Why? Because the system isn’t built to catch this.
Most electronic health records don’t flag interactions between antidepressants and decongestants. Prescribing software doesn’t warn about licorice. And patients? They don’t think a candy bar could kill them. A 2022 JAMA Internal Medicine study found that 78% of high-risk medications have inadequate warnings on their labels-especially for off-label uses.
Even worse, emergency room physicians only routinely screen for drug interactions in 35% of severe hypertension cases. That means two out of three times, the real cause is overlooked. Patients get treated for “essential hypertension,” given more pills, and sent home-only to return days later in crisis.
What Happens When It Hits
A hypertensive emergency isn’t like a heart attack with chest pain. It’s silent until it’s too late.
Signs include:
- Sudden, severe headache-often at the back of the head
- Blurred vision or seeing spots
- Chest pain or shortness of breath
- Nausea, vomiting, confusion
- Seizures or loss of consciousness
Damage can happen fast. The brain swells (hypertensive encephalopathy). The kidneys leak protein (acute kidney injury). The heart muscle strains (left ventricular hypertrophy). Retinal bleeding can cause sudden blindness. All of this can occur within hours.
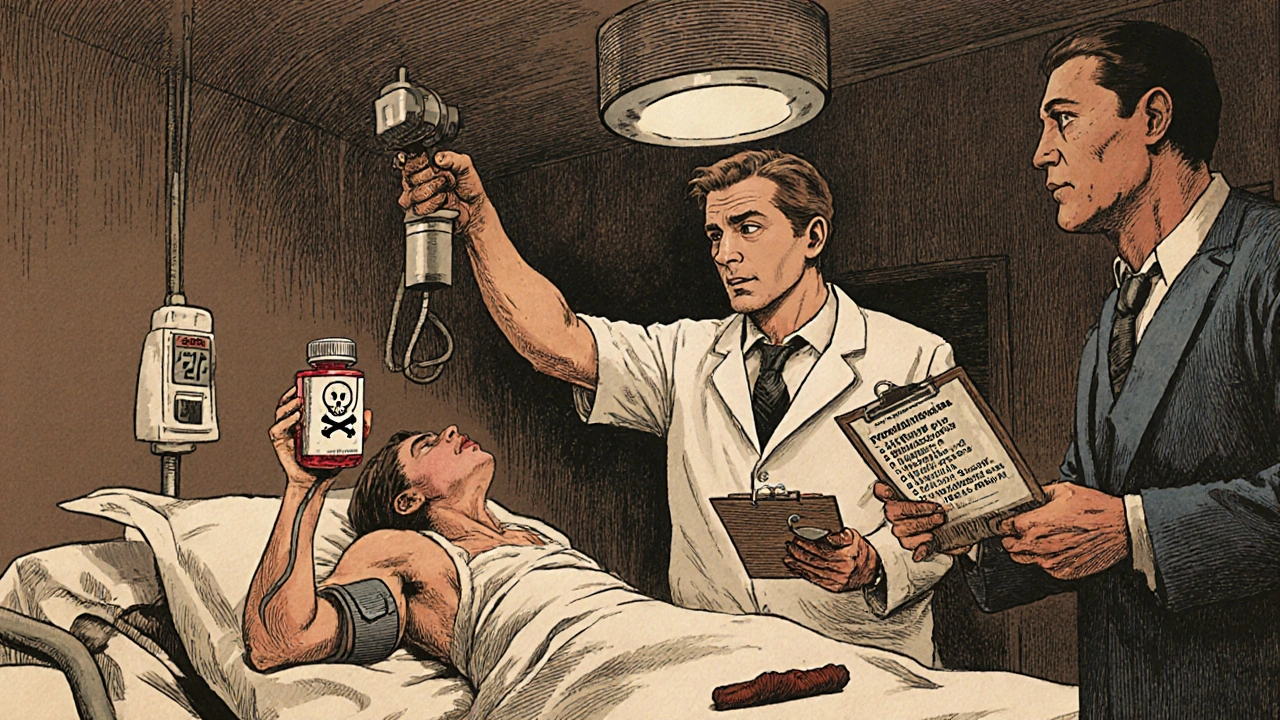
Time is critical. The goal isn’t to bring pressure down to normal overnight. It’s to reduce it by no more than 25% in the first hour-too fast, and you risk stroke. The right drugs matter too. For MAOI-related crises, intravenous phentolamine works in 92% of cases within 20 minutes. For cyclosporine-induced cases, calcium channel blockers like amlodipine are preferred. Labetalol is effective for many cases, but not all.
How to Protect Yourself
If you’re on any of these medications, here’s what you need to do:
- Know your meds. MAOIs? Avoid aged cheese, soy sauce, tap beer, cured meats, and fermented foods. Venlafaxine above 225 mg/day? Get your BP checked every 3 months. Cyclosporine? Monitor pressure weekly for the first 3 months.
- Ask before you take anything. Even “harmless” OTC meds like Sudafed, NyQuil, or Excedrin can trigger a crisis. Always check with a pharmacist.
- Track your BP at home. Buy a validated upper-arm monitor. Record readings twice a week. If you see two consecutive readings over 160/100, call your doctor.
- Use a medication checker. Apps like Medscape or Epocrates can flag interactions. The new NIH-funded AI system (in phase 3 trials) predicts 92% of high-risk interactions-but it’s not in clinics yet.
- Report adverse reactions. Use the Yellow Card system in the UK or MedWatch in the US. Your report could save someone else’s life.
One patient in Bristol traced her unexplained hypertension to daily licorice tea. She stopped. Her BP dropped 30 points in 10 days. No new meds. No hospital stay. Just awareness.
The Future Is Here-But Not Everyone’s Using It
The FDA now requires black box warnings on MAOIs. Prescription monitoring programs have cut MAOI-related crises by 28% in states with strong systems. A new AI tool, approved in early 2023, reduced MAOI emergencies by 40% in trial hospitals.
But here’s the gap: these tools aren’t mandatory. Most clinics still rely on memory and paper charts. Genetic testing for CYP2D6 enzyme variants-which can identify patients 3.2 times more likely to have severe reactions to antidepressants-isn’t routine. And with antidepressant prescriptions rising 13% yearly, and weight-loss drugs like phentermine becoming more common, the risk is climbing.
By 2027, experts predict a 35% spike in these crises. The solution isn’t just better drugs. It’s better systems. Better questions. Better patient education.
You don’t need to live in fear. But you do need to be informed. Your next cold pill might not be harmless. Your cheese sandwich might be dangerous. And your doctor might not know.
Know your meds. Ask the questions. Track your numbers. And if your pressure spikes and you feel like something’s wrong-don’t wait. Go to the ER. It could save your life.
Can over-the-counter cold medicine cause a hypertensive crisis?
Yes. Decongestants like pseudoephedrine and phenylephrine can trigger severe blood pressure spikes, especially if you’re taking antidepressants (like MAOIs or venlafaxine), beta-blockers, or have untreated hypertension. Even a single dose can cause systolic pressure to jump over 200 mmHg. Always check with a pharmacist before taking any OTC cold or allergy medication if you’re on multiple prescriptions.
Is licorice really dangerous for blood pressure?
Yes-especially black licorice. It contains glycyrrhizin, which blocks the enzyme that prevents cortisol from acting like a mineralocorticoid. This causes sodium retention, potassium loss, and fluid buildup, raising blood pressure. Just 2 ounces a day for two weeks can cause a crisis in susceptible people. Red licorice usually doesn’t contain glycyrrhizin and is safer. If you have unexplained high blood pressure, stop all licorice for two weeks and recheck your numbers.
What should I do if I accidentally eat cheese while on an MAOI?
If you’ve eaten aged cheese, cured meats, or fermented foods while on an MAOI and feel a sudden headache, chest tightness, or blurred vision, seek emergency care immediately. Do not wait. Intravenous phentolamine is the most effective treatment and works within 20 minutes. If you’re unsure, call 999 or go to the nearest ER. Even if you feel fine, monitor your blood pressure every 15 minutes for the next two hours. A delayed reaction can still occur.
Can venlafaxine cause high blood pressure even at normal doses?
At doses under 150 mg/day, venlafaxine rarely causes significant BP increases. But above 225 mg/day, the risk rises sharply. Above 300 mg/day, diastolic pressure frequently exceeds 90 mmHg. Many patients don’t realize this is a side effect-they think it’s stress or aging. If you’re on venlafaxine and your BP is rising, talk to your doctor about lowering the dose or switching medications. Quarterly BP checks are now recommended for doses above 225 mg/day.
How long does it take for blood pressure to return to normal after stopping the offending drug?
It depends on the drug. With MAOIs, stopping tyramine-rich foods can normalize pressure in 24-48 hours. With licorice, it takes 10-14 days for the body to clear glycyrrhizin. Cyclosporine-induced hypertension may take weeks to resolve, even after stopping the drug, because it alters kidney function. For cocaine or decongestants, pressure often drops within 6-12 hours. But if organ damage has occurred, recovery takes longer-and may not be complete.

Zac Gray
November 18, 2025Look, I get it-drugs can be dangerous when mixed. But let’s be real: if you’re taking MAOIs and eating cheddar like it’s popcorn, you’re not a victim of the system, you’re just ignoring the warning label that came with your prescription. I’ve seen people blame everything from licorice to their cat for their own negligence. The real issue isn’t the lack of awareness-it’s the refusal to read the damn manual. Your body isn’t a lab experiment. If you’re on something that can kill you with a snack, maybe don’t eat the snack. Simple.
Ellen Calnan
November 20, 2025I used to think hypertension was just ‘old people stuff’ until my uncle ended up in the ICU after taking Sudafed with his Zoloft. He didn’t even know they could interact. He thought ‘OTC’ meant ‘safe.’ Now he carries a card in his wallet that says ‘DO NOT GIVE ME DECONGESTANTS.’ I wish more people had that kind of clarity. You don’t need to be a doctor to save your own life-you just need to ask one question: ‘Could this kill me?’ And then actually listen to the answer.
Sam Reicks
November 20, 2025They say it’s drug interactions but what they’re really hiding is that Big Pharma wants you dependent. Licorice? A natural remedy they turned into a boogeyman. MAOIs? Designed to make you need constant monitoring so you keep buying their next pill. The system doesn’t want you healthy-it wants you docile. They don’t warn you about cheese because they profit when you end up in the ER. Look up the FDA’s funding sources. It’s not coincidence.
Marjorie Antoniou
November 22, 2025My sister was diagnosed with ‘essential hypertension’ for three years until she quit her daily licorice tea. Her BP dropped 30 points. No meds changed. Just stopped eating candy. Why isn’t this common knowledge? Why do we treat symptoms instead of looking at the whole picture? I’m not a doctor, but I know this: if something simple fixes it, why are we making it so complicated?
Michael Petesch
November 24, 2025It is noteworthy that the pharmacological literature consistently demonstrates that monoamine oxidase inhibitors, while efficacious in treatment-resistant depression, carry a well-documented risk of hypertensive crisis in the presence of tyramine-rich foods. The physiological mechanism-tyramine-induced norepinephrine release-is both robust and predictable. Yet, patient education remains inconsistent across healthcare systems. The disparity between clinical knowledge and public awareness is not merely a gap-it is a systemic failure in translational medicine.
Andrew Baggley
November 25, 2025Hey, I know this stuff sounds scary, but here’s the good news: you can take control. Get a home BP monitor. It’s like a smoke detector for your heart. Check it twice a week. If it spikes, don’t panic-just call your doc. And if you’re on antidepressants? Ask your pharmacist about OTC meds before you buy anything. Seriously. It takes two minutes. That’s two minutes that could save you a hospital stay, a family scare, or worse. You’ve got this.
Richard Risemberg
November 25, 2025I used to be a skeptic until my buddy almost died after a weekend of partying and popping propranolol with cocaine. He thought it was just ‘enhancing the high.’ He didn’t know his blood vessels were turning into pressure cookers. Now he’s a peer educator. We talk about this stuff at recovery meetings. It’s not about shaming people-it’s about giving them the facts before they become a statistic. Knowledge isn’t power-it’s survival.
Brian Rono
November 27, 2025Everyone’s acting like this is some groundbreaking revelation, but anyone who’s studied pharmacology knows this. The fact that you’re surprised means you’ve been listening to the wrong people. The medical community has been screaming about MAOI-food interactions since the 1960s. The real scandal isn’t the interaction-it’s that doctors still don’t screen for it. And now we’re blaming licorice? Please. If you think candy is the enemy, you’ve been sold a narrative. The enemy is ignorance dressed up as concern.
Steve and Charlie Maidment
November 27, 2025Okay, but let’s be honest-how many of these ‘crises’ are just people who didn’t follow instructions? I mean, if you’re on an MAOI and you eat cheese, that’s not an accident-it’s a choice. And now we’re supposed to feel bad for them? What about the people who actually follow the rules? They’re the ones getting ignored. The system isn’t broken. It’s just that some people refuse to be responsible. Stop making excuses. Read the label. It’s not that hard.
Andrew Montandon
November 27, 2025Can we just pause for a second and appreciate how wild it is that we’re still having this conversation in 2025? We have AI that can predict drug interactions with 92% accuracy… but most clinics still use paper charts? That’s like using a horse and buggy to get to the moon. And the fact that OTC meds don’t have clear warnings? That’s not negligence-that’s negligence with a corporate logo on it. I’m not mad. I’m just… disappointed. And honestly? A little scared.
Chuck Coffer
November 28, 2025Wow. So now we’re blaming cheese? Next thing you know, they’ll say water causes hypertension. You know what’s really dangerous? Trusting doctors who don’t even know what’s in their own patients’ medicine cabinets. If you’re on meds, assume everything is a threat-including your own doctor. And if you’re not paranoid? You’re not paying attention.
Frank Dahlmeyer
November 29, 2025As someone who’s worked in UK emergency services for 22 years, I’ve seen this play out too many times. A guy comes in with 240/130, sweating, terrified-says he ‘just had a cold pill.’ We check his meds: venlafaxine, 300mg. No one asked him about his OTC use. No one asked about his licorice. No one checked his diet. He was told he had ‘stress-induced hypertension.’ He came back two weeks later in cardiac arrest. The system doesn’t fail because of the drugs-it fails because of the silence. We need to ask better questions. Not just more questions. Better ones.
Codie Wagers
December 1, 2025It’s all a distraction. The real issue? The pharmaceutical-industrial complex. They don’t want you healthy. They want you on something. Always. Licorice? A scapegoat. MAOIs? A convenient villain. The truth? Blood pressure is controlled by your nervous system, your gut, your stress levels, your sleep, your trauma. But none of that makes money. So they sell you pills. And now you’re scared of cheese. Meanwhile, your cortisol is through the roof because you’re scared of cheese. The irony is delicious.