6 Jan 2026
- 9 Comments
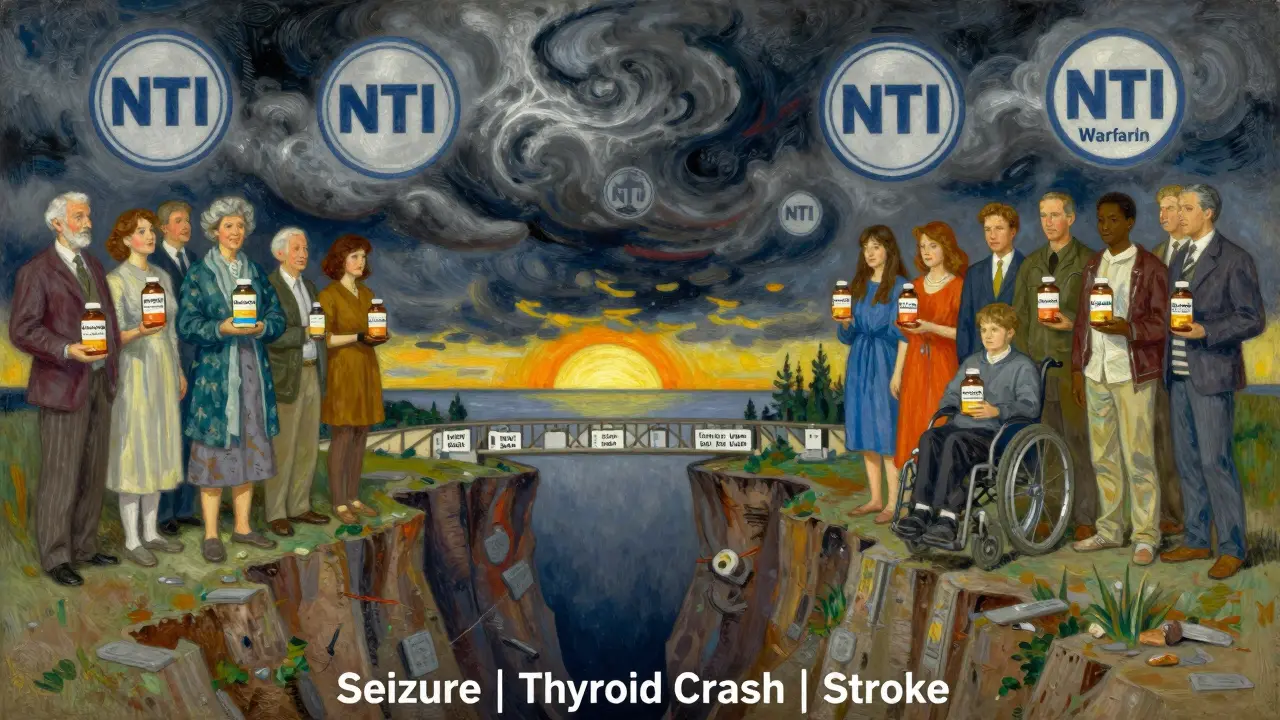
When you take a medication like levothyroxine or phenytoin, your life depends on consistency. A tiny change in dose - even a few micrograms - can mean the difference between feeling stable and having a seizure, a heart rhythm problem, or a thyroid crash. These are NTI drugs: narrow therapeutic index medications. And yet, many insurers still make patients jump through hoops to get the brand version - even when a cheaper generic is available.
What Makes NTI Drugs Different?
Not all drugs are created equal. Most medications have a wide safety margin. If you take 10% more or less than prescribed, you might feel a little off - but you won’t crash. NTI drugs don’t work that way. The FDA defines them as drugs where small differences in blood concentration can lead to serious therapeutic failure or toxicity. That’s not a guess. It’s science.
Think of it like tuning a piano. A note that’s just 5 cents off might sound slightly off to a trained ear. But for someone with epilepsy, a generic version of carbamazepine that’s 5% less potent could trigger a seizure. For someone with hypothyroidism, a switch from levothyroxine brand to generic might cause TSH levels to spike by 300%, leaving them exhausted, depressed, or at risk for heart issues.
The FDA lists about 37 drugs in this category. The big ones include:
- Levothyroxine (for thyroid disease)
- Phenytoin, carbamazepine, valproate (for epilepsy)
- Cyclosporine and tacrolimus (for organ transplants)
- Warfarin (blood thinner)
- Lithium (for bipolar disorder)
These aren’t rare drugs. Millions of Americans rely on them daily. And yet, insurers often treat them like any other medication with a generic alternative.
Why Do Insurers Demand Brand-Name NTI Drugs?
It’s not because they’re trying to be cruel. It’s because they’re trying to save money - and they think they’re being smart.
Most insurance plans push generics because they’re cheaper. That’s standard practice. But for NTI drugs, the math doesn’t add up. Studies show that when patients switch from brand to generic NTI drugs, there’s a measurable spike in hospitalizations, ER visits, and emergency interventions. One 2024 study of 2,450 epilepsy patients found that 18.7% had more seizures after being forced to switch to generics. That’s not a fluke. That’s a pattern.
Some insurers have figured this out. Health Net, for example, explicitly states in its 2023 policy that brand-name NTI drugs do not require prior authorization - even when generics exist. That’s because they’ve seen the data: the cost of a seizure or a thyroid crisis far outweighs the savings from a generic.
But not all plans are that smart. Many still require prior authorization for brand-name NTI drugs. Why? Because their systems are built for volume, not nuance. Their algorithms don’t distinguish between a blood pressure pill and a seizure medication. They just see “generic available” and lock it down.
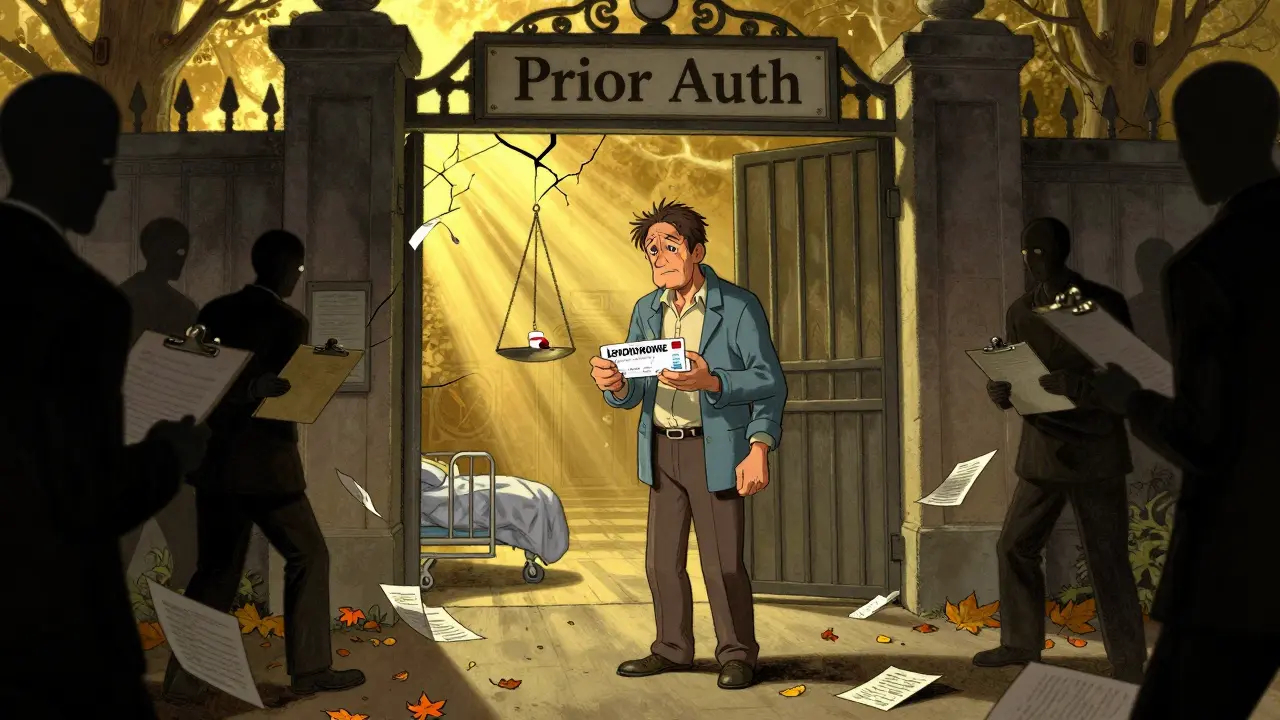
What Does Prior Authorization Actually Involve?
Prior authorization isn’t just a form. It’s a process. And for NTI drugs, it’s often a nightmare.
Here’s how it usually works:
- Your doctor prescribes the brand-name NTI drug because your condition is unstable or you’ve had bad reactions to generics.
- The pharmacy tells you the insurer won’t cover it without approval.
- Your doctor’s office spends hours filling out paperwork: lab results, TSH levels, seizure logs, weight, height, diagnosis codes.
- The request goes to the insurer’s review team - often outsourced, often understaffed.
- It takes 3 to 5 business days to get a response. Sometimes longer.
- Even if approved, you might get only a 30-day supply - and have to do it all again next month.
According to the AMCP, the goal of prior authorization is to get “additional information not available during standard claims processing.” That sounds reasonable - until you realize that for NTI drugs, that “additional information” is often the same data your doctor already has in their chart. The system doesn’t trust the doctor. It trusts a checklist.
And the cost? A 2023 MGMA survey found that physicians spend an average of 16.3 hours per week just managing prior authorizations. That’s over 800 hours a year per doctor. And for patients? A 2024 Patients Rising survey found that 68% of people taking NTI drugs faced delays longer than 72 hours. Nearly 30% reported a health event directly tied to the delay - missed doses, seizures, hospitalizations.
State Laws Are Starting to Change Things
Enough people have been hurt. Enough doctors have spoken up. And now, states are stepping in.
By January 2025, California passed AB-1428, which bans insurers from requiring prior authorization for NTI drugs if the patient was previously on the brand name and their condition is stable. No more back-and-forth. No more delays. Just continuity.
Eighteen states now require automatic approval if the insurer doesn’t respond within a set time - usually 72 hours. That’s a big deal. Before 2022, only seven states had this rule. Now, it’s growing fast.
Medicaid programs, which cover millions of low-income patients, are also shifting. Federal rules require them to respond to urgent requests within 24 hours and provide a 72-hour emergency supply. But implementation varies wildly. In North Carolina, you need a prescription that says “medically necessary.” In Mississippi, you need a special form. In some states, NTI drugs are still treated like any other drug.
The federal government is catching up too. The Improving Seniors’ Timely Access to Care Act, passed in April 2024, requires Medicare Advantage plans to give real-time electronic decisions for prior authorization - including for NTI drugs. That means no more waiting days for a response. If your doctor submits the request, you should get an answer within minutes.
What Should You Do If You’re Affected?
If you or someone you care for takes an NTI drug and keeps hitting roadblocks with insurance, here’s what to do:
- Know your drug. Is it on the FDA’s NTI list? If yes, you have grounds to push back.
- Ask your doctor to write “medically necessary” on the prescription. Some states require this for coverage.
- Use electronic prior authorization. Fax and phone calls take longer. If your doctor’s office uses a portal like NCTracks or Gainwell, insist on it. Electronic submissions are processed 42% faster.
- Appeal immediately. If your request is denied, file an appeal within 10 days. Many approvals happen on the second try - 82.4% of NTI drug prior authorizations are approved after initial denial.
- Check your state’s laws. Visit the National Conference of State Legislatures website. If your state has a law protecting NTI drug access, use it. Call your insurer and say, “I’m invoking state law [insert law number].”
- Document everything. Keep records of dates, denial letters, lab results, and how you felt when you were switched to a generic. This matters if you need to escalate to your state insurance commissioner.
The Bigger Picture: Cost vs. Safety
Insurers argue that prior authorization saves money - and they’re not wrong. One study estimated that appropriate prior authorization for NTI drugs saves health plans $2.3 billion a year. But that number doesn’t include the hidden costs: emergency room visits, hospital stays, lost workdays, caregiver time, and long-term disability.
When you force someone with epilepsy to switch generics and they have a seizure, the cost isn’t just the price of the drug. It’s the ambulance ride. The ER visit. The missed week of work. The trauma for the family.
Dr. Michael Rea of RxRevu put it bluntly: “Prior authorization for NTI drugs creates dangerous delays for patients who require immediate therapeutic consistency.” He’s not exaggerating. The data backs him up.
The trend is clear: more states are banning prior authorization for NTI drugs. More insurers are dropping it voluntarily. By 2026, analysts predict 75% of commercial plans will eliminate prior authorization for established NTI drug categories. Why? Because the risks are too high, and the backlash is too loud.
This isn’t about brand loyalty. It’s about survival. For people on NTI drugs, the difference between brand and generic isn’t a price tag. It’s a line between safety and danger.
What are NTI drugs?
NTI drugs, or narrow therapeutic index drugs, are medications where even small changes in dose or blood concentration can lead to serious side effects or treatment failure. Examples include levothyroxine, phenytoin, warfarin, and cyclosporine. These drugs have a very narrow window between being effective and being toxic.
Why do insurers require prior authorization for brand-name NTI drugs?
Many insurers require prior authorization for brand-name NTI drugs because their systems treat them like any other drug with a generic alternative - even though they’re not. The goal is to reduce costs by pushing cheaper generics. But for NTI drugs, switching can lead to dangerous health outcomes, which is why many experts and states are pushing back.
Can I get my brand-name NTI drug without prior authorization?
It depends on your insurance plan and state. Some insurers, like Health Net, don’t require prior authorization for NTI drugs at all. In states like California, laws now prohibit prior authorization if you’ve been stable on the brand. Check your state’s health policy or ask your pharmacist - many now know which drugs are exempt.
How long does prior authorization for NTI drugs take?
On average, it takes 3.2 business days for a decision. But if your request is denied, the appeal process can add more time. Electronic submissions are faster - about 42% quicker than paper. For urgent cases, some states require insurers to respond within 24 hours.
What should I do if my NTI drug request is denied?
Don’t accept the denial. File an appeal immediately - most approvals happen on the second try. Ask your doctor to submit additional clinical documentation: lab results, seizure logs, or TSH levels. If your state has a law protecting NTI drug access, cite it. You can also contact your state insurance commissioner’s office for help.

Christine Joy Chicano
January 7, 2026NTI drugs are one of those things that should’ve been obvious to insurers years ago. It’s not about brand loyalty-it’s about physics. A thyroid hormone isn’t like a painkiller where you can fudge the dose. Your body’s feedback loops are razor-thin. One microgram off, and your TSH goes from 2.5 to 7.8. Suddenly you’re exhausted, depressed, gaining 15 pounds, and your doctor says ‘it’s just adaptation.’ No. It’s pharmacology. And insurers treating this like they’re negotiating a car lease is insane.
I’ve seen patients on levothyroxine get switched to generics because the pharmacy ‘had a better deal.’ Three weeks later, they’re in the ER with atrial fibrillation. The math doesn’t lie: the cost of one hospitalization pays for a year’s supply of Synthroid. Why are we still debating this?
Adam Gainski
January 7, 2026As a pharmacist who’s filed 200+ prior auths for NTI drugs, I can tell you the system is broken. We’re not talking about some ‘maybe it works’ situation. We’re talking about patients who’ve been stable for 12 years on brand, then get switched because the formulary changed. Then they come back with tremors, confusion, or worse. The pharmacy techs don’t even know what NTI means. They just see ‘generic available’ and auto-reject.
Electronic prior auth helped a little, but the review teams are still using 2015 guidelines. If your doctor writes ‘medically necessary’ and you’ve been on the brand for 5+ years, approve it. End of story. Stop making people jump through hoops to stay alive.
Anastasia Novak
January 8, 2026Let’s be real-this is capitalism with a side of malice. Insurers don’t care if you have a seizure. They care if the generic saves them $1.27 per pill. They don’t want to hear about ‘therapeutic equivalence.’ They want to see a spreadsheet with a red arrow pointing down. And guess what? The people who pay the price aren’t the ones signing the checks.
I had a friend on warfarin get switched to generic. INR went from 2.8 to 4.9 in two weeks. She ended up with a brain bleed. The insurer’s response? ‘We followed formulary guidelines.’ You didn’t follow human guidelines. You followed profit guidelines. And that’s not just negligence. It’s criminal.
Paul Mason
January 9, 2026My uncle’s on cyclosporine after his kidney transplant. They switched him to generic last year. He got sick. Really sick. They thought it was food poisoning. Turned out his blood levels dropped 40%. He almost lost the kidney. Now they’re fighting to get him back on brand. Took three appeals, two doctors’ letters, and a call to the state insurance commissioner. It shouldn’t be this hard to stay alive.
Why do we let corporations decide who lives and who doesn’t? This isn’t healthcare. It’s a lottery.
Mina Murray
January 10, 2026Here’s the real story: the FDA lets generics pass with ±10% bioequivalence. But for NTI drugs, that’s like saying a pilot can be 10% off course and still land safely. It’s not science. It’s corporate lobbying. The same companies that make the generics also fund the FDA advisory panels. They’ve been pushing this for 20 years. You think this is about cost? It’s about control. And the patients? Just collateral damage.
steve rumsford
January 12, 2026My mom’s on lithium. They switched her to generic. She went from calm to screaming at the wall in 3 days. Took 11 days to get the brand back. She missed her job for two weeks. Now she’s on disability. I didn’t even know this was a thing until it happened to us. I thought all generics were the same. Turns out, no. Some meds are like vintage wine-you don’t swap vintages and expect the same taste.
Also, why is this even a debate? If a car part fails because you used a knockoff, you sue. Why not here?
Katrina Morris
January 14, 2026i just found out my neighbor takes phenytoin and they made her switch to generic last month. she had a seizure at the grocery store. they called 911. she was fine but scared to death. i told her to call her state rep. she didn’t know she could. i feel so bad. this is so messed up. why does it take a crisis for people to care?
also, i’m not a doctor but i googled this and it’s wild how many people are affected. we need to fix this. please.
Emma Addison Thomas
January 16, 2026I’m from the UK, and we don’t have this problem here. The NHS doesn’t play games with NTI drugs. If you’re on brand, you stay on brand. It’s not about cost-it’s about clinical responsibility. We’ve known for decades that these drugs aren’t interchangeable. Why is the US still treating this like a budget spreadsheet? We have the science. We have the data. We have the laws in some states. Why isn’t this federal policy yet?
It’s not just about money. It’s about trust. If patients can’t trust their meds, how can they trust the system?
Andrew N
January 17, 2026Everyone’s acting like this is new. It’s not. I’ve been fighting this since 2018. The data’s been out. The studies are peer-reviewed. The AMA supports it. The AAN supports it. But insurers keep dragging their feet because they’re scared of setting a precedent. If they stop prior auth for NTI drugs, what’s next? What if patients start demanding brand-name insulin? Or brand-name antibiotics? They’re afraid of the domino effect.
So they keep risking lives to protect a system that’s already failing. That’s not business. That’s cowardice.