8 Sep 2024
- 11 Comments
Calcitonin is one of those less talked-about yet vital hormones produced by the thyroid gland. Known for playing a crucial role in calcium and bone metabolism, this hormone helps to regulate blood calcium levels by inhibiting the activity of osteoclasts, the cells that break down bone.
Like many bodily functions, calcitonin levels and efficiency can vary significantly depending on age and gender. Understanding these variations is vital for maintaining good health, especially as we age. In the upcoming sections, we will explore what calcitonin is, its role in our bodies, and how its levels change with age and gender.
- What is Calcitonin?
- The Role of Calcitonin in the Body
- Age-Related Changes in Calcitonin Levels
- Gender-Specific Differences in Calcitonin Levels
- Tips for Maintaining Healthy Calcitonin Levels
What is Calcitonin?
Calcitonin, a hormone produced by the thyroid gland, plays an important role in regulating calcium levels in the blood and bone metabolism. This 32-amino acid peptide hormone is especially crucial in preventing hypercalcemia, a condition characterized by excessively high calcium levels. It acts by inhibiting the activity of osteoclasts, the cells responsible for bone resorption. By doing so, calcitonin helps in maintaining a delicate balance between bone formation and degradation.
The discovery of calcitonin marked a significant milestone in endocrinology. In 1962, researchers at the University of Oxford identified this hormone and its pivotal role in calcium and phosphate metabolism. Since then, it has been studied extensively for its potential therapeutic applications, especially in conditions like osteoporosis and Paget's disease. High calcitonin levels are often used as a biomarker for medullary thyroid carcinoma, a type of thyroid cancer.
Not many people are aware, but calcitonin is not only limited to humans. It is present in various species, including fish, birds, and mammals. The structure of the hormone is remarkably conserved across these species, emphasizing its importance in physiological processes. In fact, salmon calcitonin is often used in medical treatments because it is more potent than human calcitonin and has a longer duration of action.
"Calcitonin research has evolved remarkably, providing insights into its multifaceted roles beyond mere calcium regulation." — Dr. William Gull, Endocrinologist
Aging and gender play significant roles in modulating calcitonin levels. As people age, the secretion of calcitonin can decrease, making older adults more susceptible to bone density loss and fractures. Men and women also exhibit different calcitonin dynamics. Typically, women experience a notable decline in this hormone post-menopause, which contributes to the higher incidence of osteoporosis in older women. Understanding these nuances is vital for developing targeted treatment plans.
Calcitonin is also critical in kidney function. It aids in reducing calcium reabsorption in the kidneys, thereby promoting calcium excretion through urine. This activity helps to maintain balanced calcium levels in the blood. Emerging research suggests that calcitonin may have roles beyond bone health, including potential anti-inflammatory properties and impacts on appetite regulation. While these areas are still under investigation, the hormone’s multifaceted nature certainly makes it an intriguing subject.
Another fascinating aspect of calcitonin is its role in pregnancy. During pregnancy, calcitonin levels naturally increase to safeguard the mother’s bone density while providing adequate calcium for the developing fetus. This protective measure demonstrates the hormone's critical function in human development and maternal health. Given its wide range of activities, ongoing research into calcitonin promises to unlock even more secrets about its roles and applications in human health.
The Role of Calcitonin in the Body
Calcitonin is a hormone produced by the thyroid gland, specifically by the parafollicular cells (also known as C-cells). It plays a crucial role in regulating calcium levels in the blood. When calcium levels in the blood rise, calcitonin is released to help bring these levels down. It achieves this by inhibiting the activity of osteoclasts, the cells responsible for breaking down bone tissue.
Osteoclasts are vital for bone remodeling and repair, but their activity can also release calcium into the bloodstream. Calcitonin helps curb this process, ensuring that blood calcium levels remain within a healthy range. This regulation is crucial because calcium is needed for various bodily functions, including muscle contractions, blood clotting, and nerve transmission. Too much or too little calcium can lead to severe health issues.
The influence of calcitonin on bone health cannot be overstated. By reducing osteoclast activity, calcitonin helps to maintain bone density. This is particularly important as we age, when the risk of osteoporosis and other bone-related issues can increase. In women, the decrease in estrogen levels after menopause can lead to increased bone loss, making calcitonin’s role even more critical.
Research has shown that calcitonin also has analgesic properties, meaning it can help reduce pain. This is particularly beneficial for conditions like osteoporosis, where bone fractures can be incredibly painful. Calcitonin’s pain-relieving effects are still being studied, but preliminary results are promising.
“Calcitonin not only plays a central role in calcium homeostasis but also shows promise as a therapeutic agent for conditions involving chronic pain,” says Dr. Sarah Collins, an endocrinologist at a top medical institution.
Apart from its primary role in calcium regulation and bone health, calcitonin has been found to influence other physiological processes. For instance, some studies suggest that it may play a role in modulating appetite and body weight, although these findings are still under investigation. The hormone might interact with certain brain regions that control hunger and satiety, thereby influencing eating behaviors.
Calcitonin also has effects on the kidneys, helping to regulate the excretion of calcium and phosphate. This further contributes to its role in maintaining blood calcium levels. By increasing the amount of calcium excreted in the urine, calcitonin helps to prevent hypercalcemia, a condition characterized by excessively high calcium levels in the blood, which can be harmful.
Understanding the multifaceted role of calcitonin can lead to better insights into managing various health conditions. While its primary function is well-established, ongoing research continues to uncover new roles and potential therapeutic applications for this versatile hormone.
Age-Related Changes in Calcitonin Levels
As we journey through life, our bodies go through numerous transformations, and changes in calcitonin levels are no exception. Calcitonin plays a crucial role in maintaining calcium balance and ensuring our bones remain healthy. But how exactly do these levels fluctuate as we age?
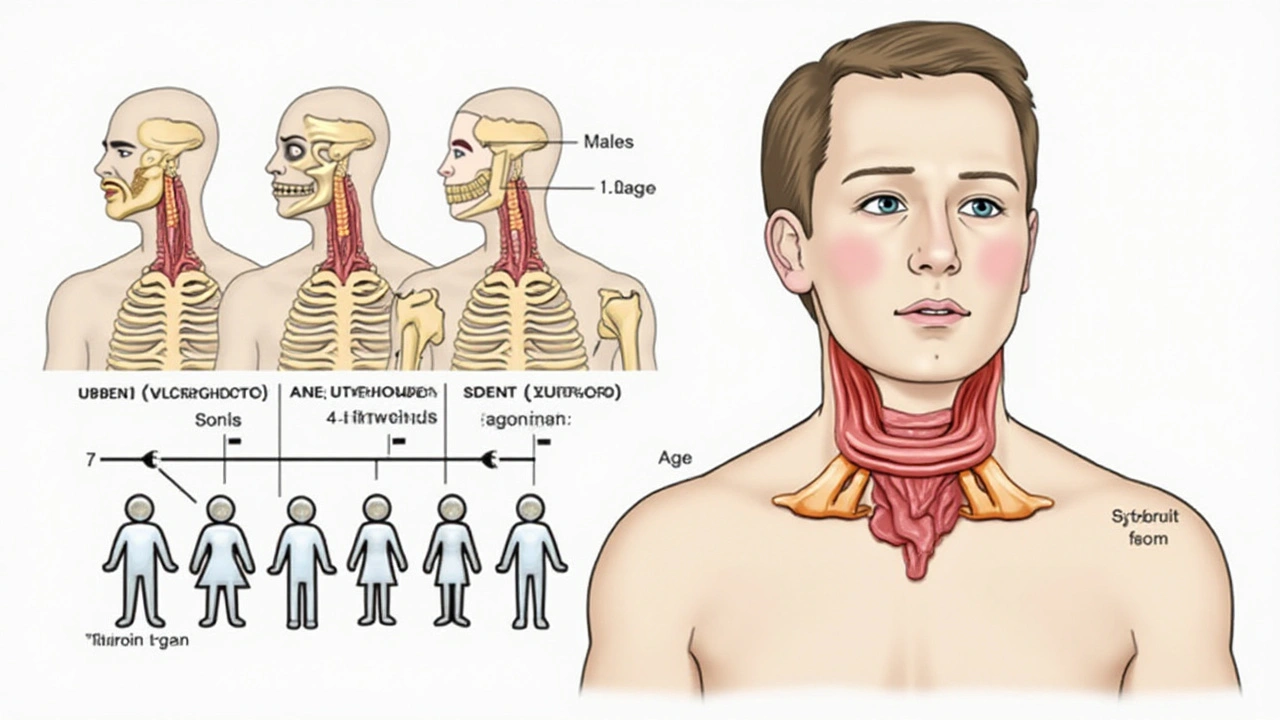
Research has shown that calcitonin levels can vary dramatically with age. During the early stages of life, calcitonin secretion is relatively high compared to later years. This increase during childhood and adolescence aligns perfectly with the rapid growth and bone development that occur during these phases. As one might expect, the high demand for calcium in growing bones necessitates a corresponding boost in calcitonin to help regulate this mineral's balance efficiently.
Once we transition into adulthood, the picture changes. Emerging evidence suggests that calcitonin levels start to decline as early as the third decade of life. This decline is gradual but noticeable and can contribute to the onset of certain age-related conditions. An interesting observation is how individuals over fifty exhibit notably lower calcitonin levels. This dip in calcitonin can impact calcium balance and bone density, often underlined as a factor in the development of osteoporosis and other bone disorders. Understanding these changes can be pivotal in preventive healthcare measures.
It's worth noting that calcitonin is not the only player in bone health and calcium regulation. It works in concert with other hormones and nutrients to maintain a delicate balance. For example, vitamin D and parathyroid hormone (PTH) are significant contributors, and their interplay with calcitonin becomes especially crucial as we age. Researchers from the Journal of Endocrinology state,
"As we age, the dynamic nature of calcium metabolism becomes more evident, with calcitonin playing a decreased yet still vital role."
In an effort to understand these shifts better, several longitudinal studies have followed participants of various ages over time, providing invaluable data. For example, a 20-year study observed individuals from their early thirties into their fifties, noting a consistent decline in calcitonin levels. The findings were clear—maintaining bone health and ensuring adequate calcium intake becomes more challenging as we age. Here, the calcitonin phenomenon plays a non-trivial role.
Interestingly, lifestyle factors can also influence calcitonin levels. People who engage in regular physical activity and maintain a balanced diet rich in calcium and vitamin D might experience a less dramatic decline. This knowledge is empowering, indicating that proactive choices can mitigate some of the natural age-related reductions in calcitonin.
Gender-Specific Differences in Calcitonin Levels
It’s fascinating how gender can influence the function and levels of calcitonin in the body. Studies have shown that calcitonin levels can vary significantly between males and females, thanks, in part, to differences in hormonal balance and metabolic needs. While both genders produce calcitonin in their thyroid glands, the quantities and efficiency can shift due to various physiological factors.
In males, testosterone appears to play a role in regulating calcitonin levels. Research suggests that men tend to have higher calcitonin levels than women, especially during their younger years. This higher level could be attributed to the anabolic effects of testosterone, which promotes bone formation and inhibits bone resorption. However, as men age and testosterone levels decrease, calcitonin levels also tend to decline, though not as sharply as in women.
Women experience unique fluctuations in calcitonin levels, heavily influenced by estrogen. During their reproductive years, estrogen promotes the production of calcitonin, which helps to maintain healthy bones and adequate calcium balance. Interestingly, postmenopausal women often see a dramatic drop in both estrogen and calcitonin levels, which can lead to an increased risk of osteoporosis. This drop is one reason why bone fractures are more common among older women.
“The relationship between estrogen and calcitonin is pivotal for bone health, particularly in postmenopausal women,” notes Dr. Harriet Meade, a renowned endocrinologist.
Another intriguing aspect is how pregnancy affects calcitonin levels in women. During pregnancy, there is an increased demand for calcium to support the developing fetus. Consequently, calcitonin levels often rise to meet this increased need, helping to ensure that both the mother and the baby maintain sufficient calcium levels.
In both men and women, lifestyle factors like diet and physical activity can also impact calcitonin levels. A diet rich in calcium and regular weight-bearing exercise may help to sustain healthy calcitonin production. These habits are especially important for women approaching menopause. Smoking and excessive alcohol consumption, on the other hand, can adversely affect calcitonin levels and should be limited.
A recent study published in the Journal of Clinical Endocrinology & Metabolism found that men who maintained an active lifestyle throughout middle age had a lesser decline in calcitonin levels compared to their sedentary counterparts. This study highlights the importance of physical activity in the aging process, irrespective of gender.
| Factor | Impact on Calcitonin Levels |
|---|---|
| Gender | Males generally have higher levels |
| Hormones | Testosterone in men & Estrogen in women |
| Age | Levels decline with age in both genders |
| Pregnancy | Increases levels in women |
Understanding these gender-specific differences in calcitonin levels can aid in targeted approaches to maintaining bone health. Whether it's through hormone replacement therapy, diet, or exercise, individual strategies might be required to optimize calcitonin levels effectively.

Tips for Maintaining Healthy Calcitonin Levels
Maintaining healthy calcitonin levels is not only important for strong bones but also for the efficient regulation of blood calcium. As we age, our bodies undergo various changes that can affect the production and secretion of hormones like calcitonin. Likewise, gender differences can play a subtle role in how our bodies handle this vital hormone. Here are some actionable tips to help keep your calcitonin levels in check.
Nutrition and Diet
Your diet plays a critical role in maintaining adequate calcitonin levels. Make sure to include foods that are rich in calcium, such as dairy products, leafy green vegetables, and fortified cereals. Calcium is a key player in bone density and the prevention of osteoporosis, a condition that calcitonin helps to mitigate. In addition to calcium, ensure you're getting enough vitamin D, as it aids in calcium absorption.
- Calcium-Rich Foods: Milk, cheese, and yogurt
- Leafy Greens: Spinach, kale, and broccoli
- Fortified Cereals: Options with added calcium and vitamin D
Exercise and Physical Activity
Regular physical activity is crucial for maintaining healthy hormone levels, including calcitonin. Weight-bearing exercises, like walking, running, and resistance training, can help strengthen bones and boost calcitonin production. Aim for at least 150 minutes of moderate-intensity exercise per week, coupled with strength training sessions at least twice a week.
"Regular physical exercise can have a profound impact on hormone levels and overall bone health." — A renowned endocrinologist
Avoid Excessive Alcohol and Smoking
Alcohol and smoking can have detrimental effects on your overall health, including your calcitonin levels. Excessive alcohol consumption has been linked to lower bone density, while smoking can interfere with the body's ability to absorb calcium and produce calcitonin. Try to limit your alcohol intake and quit smoking if you haven't yet taken that step.
Regular Medical Check-Ups
Regular visits to your healthcare provider can help monitor your hormone levels, including calcitonin. Blood tests can provide insights into how well your thyroid is functioning. If your calcitonin levels are off, your doctor can offer personalized advice and treatments to correct any imbalance. Early detection and intervention are often key to maintaining good health.
Supplements and Medication
Sometimes, diet and exercise might not be enough to keep your calcitonin levels within the optimal range. In such cases, your healthcare provider might recommend supplements or medications. Calcium and vitamin D supplements are commonly advised, especially for older adults. If there's a significant issue with your thyroid function, specific medications might be necessary to regulate hormone levels.
By following these tips, you can take proactive steps to ensure that your calcitonin levels remain balanced, thereby supporting your bone health and overall well-being. Keep in mind that a holistic approach involving diet, exercise, lifestyle changes, and regular medical care is often the most effective way to maintain your health as you age.

jake cole
September 9, 2024Calcitonin levels dropping with age is just another excuse for the pharma industry to push cheap supplements.
Natalie Goldswain
September 19, 2024i think adding kale and milk daily helps keep that calcitonin thing steady.
khajohnsak Mankit
September 28, 2024The dance of calcium and calcitonin is akin to a silvery thread weaving through the tapestry of our bones, each tug echoing the silent whispers of hormonal balance. As we age, the loom slows, and the thread thins, revealing the fragility beneath. Yet, it isn’t merely a decline; it is a symphony of endocrine dialogues, where estrogen and testosterone converse with the thyroid’s C‑cells. Understanding this choreography invites us to intervene with diet and movement, lest the canvas crumble. In short, honoring the rhythm of our hormones may keep the masterpiece intact.
Jayant Paliwal
October 8, 2024Analyzing calcitonin trends is not merely a statistical exercise; it is a moral imperative, demanding that we scrutinize every datum with unforgiving rigor. The decline observed in elderly populations, for instance, cannot be dismissed as inevitable-rather, it highlights systemic neglect, an oversight that the medical establishment must rectify. Moreover, gender disparities, while biologically plausible, are often exaggerated by sensationalist media, thereby skewing public perception. One must ask whether the prevailing therapeutic protocols genuinely address the underlying endocrine shifts or merely apply a one‑size‑fits‑all remedy. In my view, the literature suffers from confirmation bias, selecting studies that affirm preconceived notions while ignoring contradictory evidence. Consequently, clinicians should adopt a more nuanced, evidence‑based approach, integrating hormonal profiling with individualized lifestyle interventions. Ultimately, the integrity of endocrinology hinges upon our willingness to challenge complacency and demand methodological excellence.
Kamal ALGhafri
October 17, 2024When we consider calcitonin’s role, it becomes evident that the hormone is a quiet guardian of skeletal integrity. Age‑related declines should prompt us to reflect on lifestyle choices rather than resign to destiny. Both men and women can mitigate the drop through adequate calcium intake and weight‑bearing exercise. Moral responsibility lies in educating the public before pathology takes hold.
Gulam Ahmed Khan
October 27, 2024Totally agree – a daily walk plus a glass of milk can keep those levels humming! 😊 Keep it up and your bones will thank you.
John and Maria Cristina Varano
November 5, 2024the article miss some key data its all to basic and i cant beleive they left out the 2020 study on indian men its obvious the researchers are slacking.
Melissa Trebouhansingh
November 15, 2024While the preceding observation offers a commendable layperson’s perspective, one must also acknowledge the profound epistemological implications embedded within calcitonin’s endocrine modulation. The subtle interplay between osteoclastic inhibition and renal calcium excretion, though often oversimplified, warrants a rigorous scholarly discourse that transcends superficial salutations. Moreover, the gender‑specific hormonal milieu-particularly the precipitous post‑menopausal decline-beckons an interdisciplinary nexus of endocrinology, gerontology, and sociocultural analysis. Hence, the pursuit of a holistic therapeutic paradigm remains an exigent scholarly imperative.
Brian Rice
November 25, 2024The hormonal landscape described herein demands a meticulous appraisal grounded in evidence‑based medicine. Calcitonin’s physiological decline with advancing age is a phenomenon well‑documented across longitudinal cohorts. Such diminution, however, does not operate in isolation; it intertwines with concomitant alterations in parathyroid hormone and vitamin D metabolism. The resultant net effect on calcium homeostasis may predispose the elderly to osteoporotic fractures if unmitigated. Gender differentials further complicate this tableau, given that estrogenic attenuation in post‑menopausal women accelerates the loss of calcitonin efficacy. Clinical practice guidelines therefore endorse routine monitoring of serum calcium and calcitonin levels, particularly in high‑risk demographics. Therapeutic strategies may incorporate calcium‑rich nutrition, vitamin D supplementation, and weight‑bearing exercise regimens. In certain clinical contexts, synthetic salmon calcitonin analogues have demonstrated analgesic benefits alongside bone‑preserving effects. Nonetheless, the utility of such pharmacologic agents must be weighed against potential adverse events, including nausea and hypersensitivity reactions. Beyond pharmacotherapy, lifestyle modifications remain the cornerstone of preventive care. Regular physical activity stimulates osteoblastic activity, thereby counterbalancing osteoclastic suppression mediated by calcitonin deficits. Additionally, avoidance of excessive alcohol consumption and tobacco use preserves vascular health, indirectly supporting skeletal robustness. It is incumbent upon healthcare providers to deliver personalized education that integrates these multifaceted considerations. Ultimately, a comprehensive, patient‑centred approach offers the greatest prospect for mitigating age‑related calcium dysregulation and preserving skeletal integrity.
Stan Oud
December 4, 2024One could argue that the above discourse is overly detailed-sometimes brevity serves clarity; however, nuance is essential. Still, the core message remains: proactive measures matter.
Ryan Moodley
December 14, 2024In the grand theater of endocrinology, calcitonin takes its place as both sentinel and supplicant-guarding calcium while pleading for attention. Yet many overlook its subtle power, focusing instead on louder hormonal voices. Recognizing its quiet influence may reshape how we approach bone health across the lifespan.