29 Jan 2026
- 12 Comments
For many people, a stuffy nose that won’t go away isn’t just annoying-it’s exhausting. If you’ve had blocked sinuses, facial pressure, or a dull sense of smell for more than three months, you’re not just dealing with a bad cold. You might have chronic sinusitis, a condition that affects nearly 1 in 10 adults worldwide. Unlike a regular sinus infection that clears up in a couple of weeks, this one sticks around, often despite antibiotics, decongestants, or home remedies. The truth? It’s rarely about bacteria. It’s about inflammation, anatomy, and triggers you might not even realize you’re exposed to every day.
What Chronic Sinusitis Really Feels Like
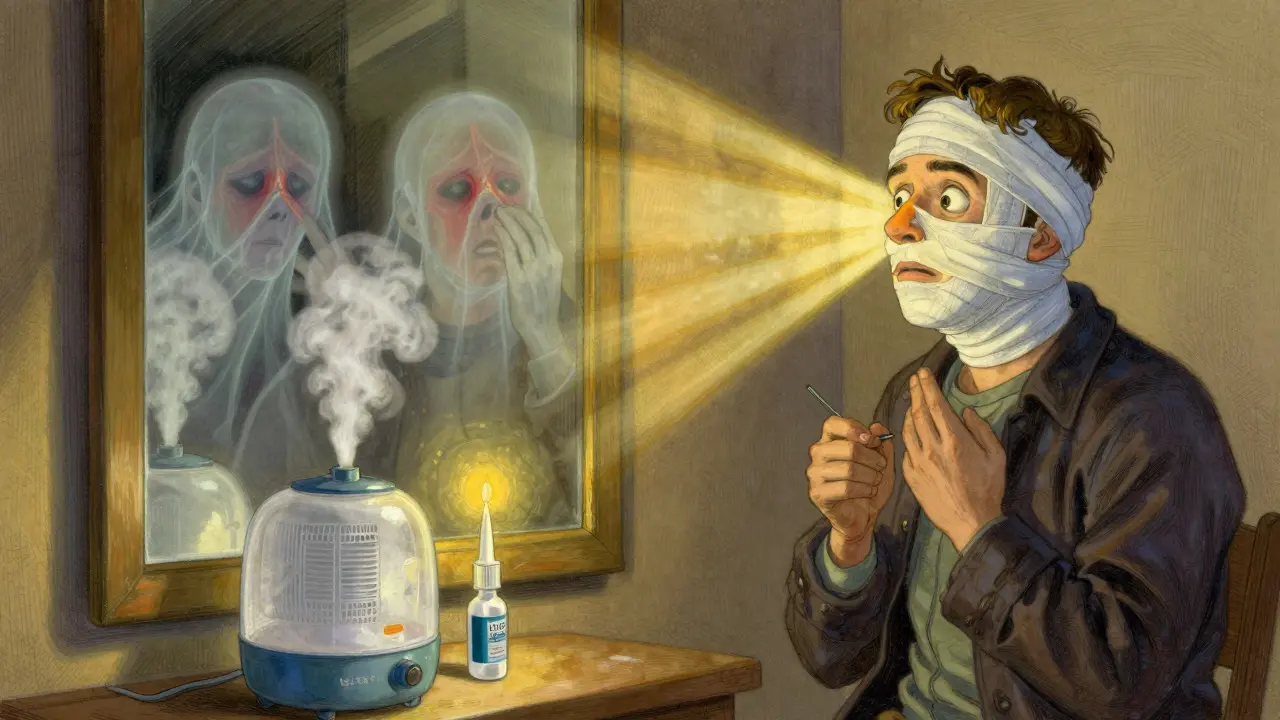
Imagine waking up every morning with your nose feeling like it’s stuffed with cotton. Breathing through it feels like trying to suck air through a straw. Your face aches, especially around your eyes and cheeks, and your throat is constantly coated in thick mucus you can’t seem to clear. Your sense of smell? Gone. Food tastes bland. You’re tired all the time. And no matter how much you blow your nose, nothing changes.
This is chronic sinusitis-or chronic rhinosinusitis, as doctors call it. The official diagnosis requires at least two of these symptoms lasting 12 weeks or longer: nasal blockage, thick nasal discharge (front or back), facial pain or pressure, and loss of smell. You might also have headaches, ear pressure, or a cough that won’t quit. What makes it worse is that you’ve probably tried everything: steam inhalers, neti pots, over-the-counter sprays, even antibiotics. And yet, it’s still there.
It’s not just a physical burden. People with chronic sinusitis report trouble sleeping, difficulty concentrating at work, and avoiding social events because they feel self-conscious about breathing loudly or having a runny nose. Studies show that 65% of patients say it interferes with their daily life-more than many other chronic conditions.
It’s Not Just an Infection
Most people think sinusitis means bacteria. That’s true for acute cases-those quick, painful infections that follow a cold. But chronic sinusitis? It’s rarely about active infection. In fact, about 70% of cases have no live bacteria causing the problem. Instead, it’s your body’s own immune system overreacting.
Think of it like a fire alarm that won’t stop ringing. Your sinuses are inflamed because something is constantly triggering them. The most common triggers? Allergies, nasal polyps, and environmental irritants.
If you have hay fever, asthma, or eczema, your risk of chronic sinusitis jumps by 2.5 to 4 times. Why? Because your immune system is already on high alert. Pollen, dust mites, pet dander-these don’t just make you sneeze. They set off a chain reaction in your nasal lining, causing swelling and mucus buildup that blocks the tiny drainage channels in your sinuses.
Nasal polyps-soft, noncancerous growths inside your nose-are another major player. They’re present in about 1 in 4 people with chronic sinusitis. These polyps aren’t painful, but they’re like roadblocks. They physically block airflow and trap mucus, making infections more likely and healing nearly impossible.
And then there’s the environment. Smoking, air pollution, chemical fumes, even dry indoor air from heating systems can irritate your nasal lining. One study found that exposure to tobacco smoke increases your risk by 35%. If you live in a city with poor air quality or spend hours in an air-conditioned office, you’re adding fuel to the fire.
How Doctors Diagnose It-And Why It’s Not Just a Look and a Guess
Many patients are misdiagnosed because their doctor assumes it’s a bacterial infection and prescribes antibiotics. That’s why so many people feel like nothing works. A real diagnosis requires more than a quick glance.
Doctors use two key tools: nasal endoscopy and CT scans. Endoscopy involves a thin, flexible tube with a camera that’s inserted into your nose. It lets the doctor see exactly what’s going on-swelling, pus, polyps, or a deviated septum. A CT scan gives a detailed 3D image of your sinuses, showing which ones are blocked or thickened with mucus.
There are three main subtypes, and knowing which one you have changes your treatment plan:
- Chronic sinusitis without nasal polyps-Most common. Often tied to allergies or environmental triggers.
- Chronic sinusitis with nasal polyps-Harder to treat. Requires stronger anti-inflammatory approaches.
- Allergic fungal rhinosinusitis-Rare. Happens when fungi trigger a severe allergic reaction in the sinuses. More common in warm, humid climates.
Without this level of detail, treatment is just guessing. And guessing doesn’t fix chronic sinusitis.
First-Line Treatment: It’s Not What You Think
Forget antibiotics. The real first-line treatment? Saline rinses and steroid nasal sprays. That’s it. And yes, it’s that simple-when done right.
Nasal saline irrigation (using a neti pot or squeeze bottle with sterile salt water) flushes out irritants, allergens, and thick mucus. It’s cheap, safe, and works for most people. Studies show that when used daily, it improves symptoms in over 70% of patients within a few weeks.
Then comes the nasal corticosteroid spray. These aren’t the same as the oral steroids you might have heard about. These are targeted, low-dose sprays that reduce swelling right where it matters. Common brands include Flonase (fluticasone), Rhinocort (budesonide), and Nasonex (mometasone). They don’t work overnight. It takes 4 to 8 weeks of daily use to see real results. But if you stick with them, 60-70% of people get significant relief.
And here’s the catch: most people stop using them too soon. Only about 60% of patients use their spray consistently. Why? Because it feels weird at first. Some get nosebleeds. Others don’t feel better right away and give up. But stopping early is why so many think it doesn’t work. Consistency is everything.
If allergies are the main driver, antihistamines like loratadine or cetirizine can help. They don’t fix the inflammation, but they reduce sneezing and runny nose, making other treatments more effective.
When Medication Isn’t Enough: Biologics and the New Frontier
For those with severe chronic sinusitis-especially with nasal polyps-traditional treatments often fall short. That’s where biologics come in. These are not pills or sprays. They’re injections that target specific parts of your immune system.
Dupilumab (Dupixent) was approved in 2019 specifically for chronic sinusitis with nasal polyps. In clinical trials, it reduced polyp size by 50-60% and improved breathing and smell in 30-40% of patients. It’s not a cure, but for many, it’s life-changing. You get a shot every two weeks, and within months, you can breathe through your nose again.
Other biologics like omalizumab (Xolair) and mepolizumab (Nucala) are also being used off-label with success. They’re expensive-often over $10,000 a year-but many insurance plans cover them if you’ve tried everything else.
There’s also aspirin desensitization for people with Samter’s triad-those who have asthma, nasal polyps, and are sensitive to aspirin. It sounds strange, but under medical supervision, slowly increasing doses of aspirin can reduce polyp growth and inflammation by 70-80% over time.
And research is moving fast. Early studies at Johns Hopkins are testing probiotics in the nose to rebalance the sinus microbiome. Early results show a 30-40% reduction in inflammation for some patients. It’s not mainstream yet, but it’s coming.
Surgery: When It’s the Right Choice
If you’ve tried daily saline rinses, steroid sprays, antihistamines, and even biologics-and you’re still struggling-surgery might be the next step. But it’s not a last resort. It’s a tool. And it works best when paired with ongoing medical care.
Functional Endoscopic Sinus Surgery (FESS) is the gold standard. It’s not open surgery. It’s done through the nose using a tiny camera and instruments. The surgeon removes blockages, opens up the sinuses, and improves drainage. Success rates? 75-90% of patients report major improvement. Recovery takes about a week. You might have some crusting or mild bleeding, but no external scars.
There’s also balloon sinuplasty. It’s less invasive. A small balloon is inflated inside the blocked sinus to widen it. Recovery is faster-3 to 5 days. But it’s not as effective for severe cases or large polyps. Think of it as a temporary fix, not a permanent solution.
If you have nasal polyps, a polypectomy (removing the polyps) is often done at the same time as FESS. It gives quick relief, but without ongoing steroid sprays, polyps come back in 40-50% of cases within 18 months.
And if you have a deviated septum? A septoplasty can be done alongside sinus surgery. It helps with airflow and can improve the success of other treatments. About 70% of patients with both conditions report better breathing after combined surgery.
Long-Term Management: It’s a Lifestyle, Not a Cure
Chronic sinusitis isn’t something you fix and forget. It’s a condition you manage. And that means daily habits matter more than you think.
- Use a humidifier in dry months. Dry air dries out your nasal lining, making it more prone to irritation.
- Avoid smoking and secondhand smoke. Period.
- Wash your bedding weekly in hot water to kill dust mites.
- Use HEPA filters in your bedroom and vacuum cleaner.
- Stay hydrated. Thinner mucus drains better.
- Don’t skip your steroid spray-even when you feel fine. Prevention is the goal.
Many patients who stick with this routine report a 50% drop in flare-ups. It’s not glamorous. But it works.
What Happens If You Ignore It?
Most people worry about complications. The truth? Serious ones are rare-less than 0.5% of cases. But they’re serious. Infection can spread to your eyes, bones, or even your brain. That’s why persistent symptoms need attention, not just waiting it out.
More common? Constant fatigue, poor sleep, anxiety from never feeling well, and missing work or school. Your quality of life slowly erodes. That’s why early, consistent treatment matters more than waiting for something to get worse.
Is chronic sinusitis caused by bacteria?
Not usually. While acute sinus infections are often bacterial, chronic sinusitis is primarily an inflammatory condition. About 70% of cases involve allergies, nasal polyps, or environmental triggers-not active infection. Antibiotics rarely help unless there’s a clear bacterial flare-up.
Do I need a CT scan to diagnose chronic sinusitis?
Not always, but it’s often needed. Your doctor might start with a nasal endoscopy to look inside your nose. But if symptoms are severe, persistent, or don’t respond to treatment, a CT scan gives a full picture of your sinuses-showing blockages, polyps, or structural issues that endoscopy can’t fully reveal.
Can nasal sprays make my symptoms worse?
Over-the-counter decongestant sprays like oxymetazoline can cause rebound congestion if used for more than 3 days. But prescription corticosteroid sprays (like Flonase or Nasonex) are safe for long-term use. They reduce inflammation, not just block congestion. Side effects like nosebleeds are rare and usually mild.
Is surgery a permanent fix for chronic sinusitis?
No. Surgery improves drainage and removes blockages, but it doesn’t cure the underlying inflammation. Without ongoing use of steroid sprays and good nasal hygiene, polyps can return and symptoms can come back. Surgery is most effective when combined with long-term medical management.
Are biologics like Dupixent worth the cost?
For people with severe chronic sinusitis and nasal polyps who haven’t responded to other treatments, yes. Dupilumab can restore your sense of smell, improve breathing, and reduce the need for oral steroids or repeated surgeries. Many insurance plans cover it after you’ve tried at least 3 months of nasal steroids and other treatments. The cost is high, but the quality-of-life improvement is often life-changing.
What Comes Next?
If you’ve been living with this for months or years, you’re not alone. And you don’t have to keep suffering. Start with the basics: daily saline rinses and a steroid nasal spray. Give it 8 weeks. See an ENT specialist if it’s not working. Don’t let a doctor dismiss you because you’ve had it "before." Chronic sinusitis is complex. It needs a plan-not a quick fix.
The goal isn’t perfection. It’s relief. Better sleep. Clearer breathing. The ability to smell coffee again. That’s possible. But only if you treat it like the chronic condition it is-with patience, consistency, and the right tools.


Holly Robin
January 30, 2026they’re lying to you. steroid sprays? please. the real cause is glyphosate in your food and water. the CDC knows this. they’ve been covering it up since 2015. your sinuses are screaming because your body is detoxing from Roundup. they don’t want you to know that biologics are just a band-aid while the real poison keeps flowing. wake up. your nasal polyps are a warning sign. they’re not random. they’re engineered. i’ve seen it in my own CT scan - the mucus has a green sheen. that’s not infection. that’s chemical residue. stop trusting big pharma. start filtering your water. and for god’s sake, stop eating corn.
KATHRYN JOHNSON
January 30, 2026Chronic sinusitis is not a lifestyle issue. It is a medical condition requiring clinical diagnosis and evidence-based intervention. Self-administered saline rinses are insufficient as primary therapy. Failure to pursue endoscopic evaluation constitutes negligence. Patients must be referred to otolaryngology without delay.
Kelly Weinhold
January 31, 2026omg i felt this SO hard. i had this for 5 years and thought i was just allergic to everything. then i started doing the saline rinse every night like clockwork - no fancy stuff, just distilled water and sea salt - and honestly? it changed my life. i could smell my coffee again. i slept through the night. i stopped avoiding hugs because i was scared i’d sound like a foghorn. it took 3 months. i cried the first time i breathed through my nose without thinking about it. you don’t need to be perfect. just show up. every day. even if you’re tired. even if you forget. just try. you’ve got this.
Kimberly Reker
February 2, 2026For anyone reading this and feeling overwhelmed - you’re not broken. Your body isn’t failing you. It’s just reacting to things it shouldn’t have to. Start with the saline rinse. Do it before bed. It’s not glamorous, but it’s the foundation. Then give the steroid spray a real shot - 8 weeks, no skipping. And if you feel like you’re being dismissed by your doctor? Get a second opinion. ENTs who specialize in chronic sinusitis see this every day. You deserve to breathe.
Eliana Botelho
February 4, 2026Okay but have you considered that maybe the whole concept of "chronic sinusitis" is just a capitalist scam to sell you sprays and surgeries? I mean, think about it - if it was really about inflammation, why do people in rural areas with zero access to healthcare never have this? It’s all about exposure to modern life. Air conditioning. Processed food. Plastic containers. Even your phone screen emits something that messes with your nasal cilia. I stopped using deodorant and switched to bamboo pillows and my symptoms vanished. No meds. No surgery. Just woke up one day and realized I hadn’t blown my nose in three weeks. Coincidence? I think not.
Rob Webber
February 4, 2026Biologics cost $10,000 a year? That’s a joke. The system is rigged. You’re supposed to suffer quietly until you’re rich enough to afford relief. Meanwhile, people in the Midwest are still getting antibiotics for this like it’s 2005. And don’t get me started on how ENTs treat patients like they’re inconveniencing them. I had to beg for a CT scan. They said "it’s probably just allergies." I had polyps the size of grapes. They didn’t even look. I’m not asking for sympathy. I’m asking for accountability.
calanha nevin
February 4, 2026Consistent saline irrigation and intranasal corticosteroids remain the cornerstone of management. Biologics are indicated for severe disease with polyps refractory to standard therapy. Surgery improves anatomical obstruction but requires long-term medical adherence to prevent recurrence. The data is clear. The challenge is adherence. Patient education is not optional. It is essential.
Lisa McCluskey
February 6, 2026My mom had this for 20 years. She tried everything. Then she started using a humidifier at night and washing her sheets weekly. No drama. No supplements. Just simple habits. She still uses the spray but doesn’t panic when she has a bad day. It’s not about being cured. It’s about living with it without letting it own you. You’re not alone.
Niamh Trihy
February 7, 2026Interesting that you mention the microbiome research. I’ve been using a nasal probiotic spray from a clinical trial in Dublin. Not FDA approved yet, but my sense of smell improved after 6 weeks. Still using my steroid spray, but the constant post-nasal drip? Gone. It’s not magic. But it’s promising. If you’re curious, ask your ENT about the Dublin trial - they’re still recruiting.
Jason Xin
February 8, 2026So you’re telling me the real cure is doing nothing for two months while you wait for a spray to work? And we’re supposed to believe that’s better than just popping an antibiotic? The irony is thick enough to choke on. But hey, if you’re okay with waiting and bleeding from your nose for 8 weeks, more power to you. I’ll take the pill that works in three days, thanks.
Blair Kelly
February 8, 2026Biologics are not a cure. They’re a temporary fix for a broken system. The real issue? No one’s addressing the root cause: environmental toxins. The air in this country is toxic. The water is laced with endocrine disruptors. The food is chemically altered. This isn’t medicine. This is damage control. And the doctors? They’re just the janitors cleaning up the mess they helped create.
Gaurav Meena
February 9, 2026As someone from India who’s lived with this since childhood, I can say - this article is spot on. We don’t have access to biologics here, but saline rinses and steam with eucalyptus? Life-changing. And yes, the polyps come back if you stop the spray. But I’ve learned to treat it like brushing my teeth - daily, non-negotiable. I’m 34 and finally feel like I can live, not just survive. You got this. Keep going.