18 Oct 2025
- 14 Comments
Prednisolone Interaction Checker
Select medications you are taking alongside prednisolone to check for potential interactions
Select a medication to see interaction information
When taking Prednisolone is a synthetic glucocorticoid used to reduce inflammation and suppress the immune system, you’ll quickly discover that not every pill plays nicely with it. Prednisolone interactions can turn a routine prescription into a health hiccup, so knowing which medicines to steer clear of is essential for staying on track.
Key Takeaways
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) raise the risk of stomach ulcers and bleeding.
- Anticoagulants such as warfarin become more potent, requiring closer monitoring.
- Certain antifungals (e.g., ketoconazole) and antibiotics (e.g., clarithromycin) boost prednisolone levels, increasing side‑effects.
- Live vaccines may be less effective while you’re on prednisolone, so timing matters.
- Rifampin and some anticonvulsants speed up prednisolone clearance, potentially lowering its benefit.
How Prednisolone Works
Prednisolone mimics the body’s natural cortisol, binding to glucocorticoid receptors in almost every cell. This binding shuts down inflammatory pathways, slows immune‑cell activity, and influences metabolism. Because it touches so many systems, any other drug that changes liver enzymes, blood clotting, or immune response can tip the balance-sometimes dramatically.
Why Interactions Matter
Glucocorticoids already come with a laundry list of possible side‑effects: high blood sugar, bone loss, mood swings, and increased infection risk. When another medication interferes, those risks can intensify, or the intended therapeutic effect can disappear. That’s why doctors always ask for a full medication list before starting prednisolone.
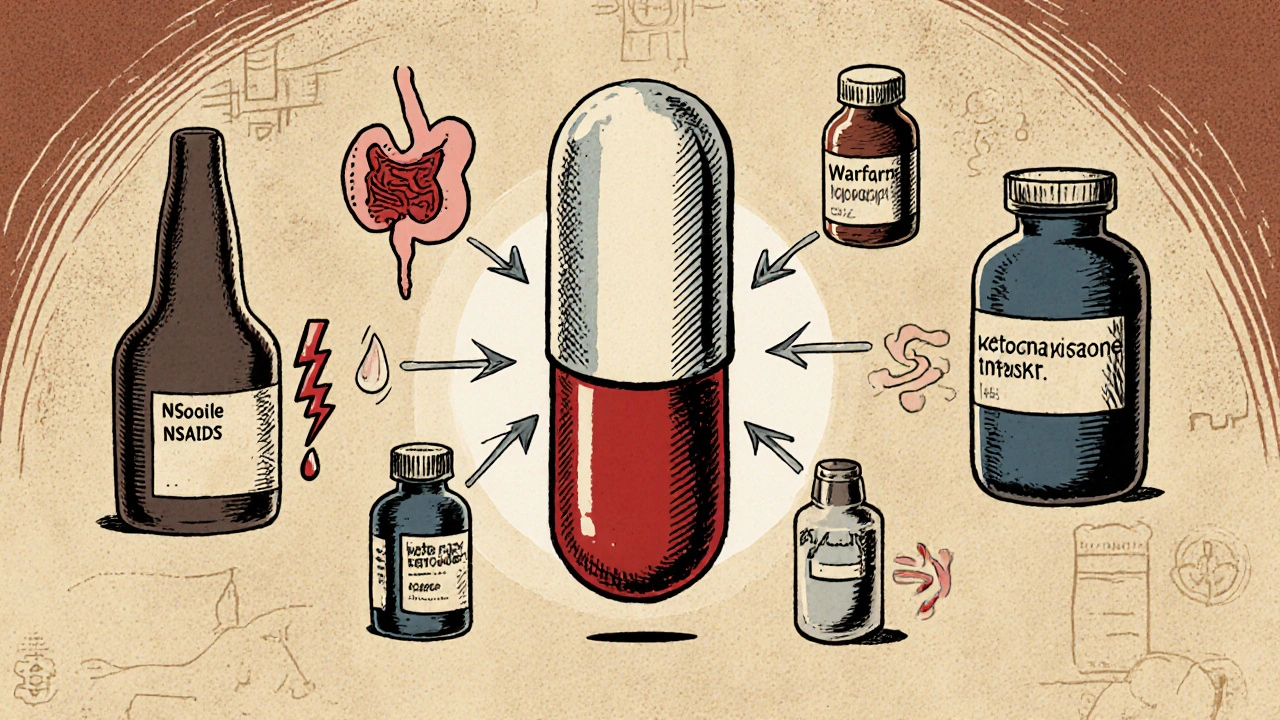
Medications to Avoid or Use With Caution
Below are the main drug families that commonly clash with prednisolone. For each, we explain what happens, why it matters, and how you can stay safe.
Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs)
NSAIDs are a class of pain relievers that also thin the stomach lining. When paired with prednisolone, they double‑dip on gastrointestinal irritation, heightening the chance of ulcers or bleeding. If you need pain relief, acetaminophen is usually gentler, but always check with your prescriber.
Anticoagulants
Warfarin is a vitamin K antagonist that thins the blood. Prednisolone can boost its effect by increasing clotting factor sensitivity, so INR (international normalized ratio) may jump unexpectedly. Regular blood tests become crucial, and dose adjustments might be needed.
Antifungal and Antibiotic Boosters
Ketoconazole is a potent CYP3A4 inhibitor used for fungal infections. It blocks the enzyme that clears prednisolone, leading to higher steroid concentrations and a higher chance of mood changes, high blood pressure, or glucose spikes. The same story applies to Clarithromycin, a macrolide antibiotic that also inhibits CYP3A4.
Enzyme Inducers
Rifampin is a CYP3A4 inducer commonly used for tuberculosis. It speeds up prednisolone metabolism, potentially dropping its anti‑inflammatory power. If you’re on rifampin, your doctor may raise the prednisolone dose or switch to a different steroid.
Antiretrovirals
Ritonavir is a CYP3A4 inhibitor used in HIV therapy. Like ketoconazole, it can push prednisolone levels up, so close monitoring for steroid‑related side‑effects is advised.
Live Vaccines
Vaccines that contain weakened viruses-such as the varicella or yellow‑fever shots-rely on a functional immune system to create protection. Prednisolone dampens immunity, meaning the vaccine may not work well and, in rare cases, could cause infection. Schedule vaccinations before starting a high‑dose course or ask your doctor about timing.
Diabetes Medications
Prednisolone raises blood‑sugar levels. If you’re on metformin or other glucose‑lowering drugs, you may need a temporary dose increase while on steroids. Frequent glucose checks help keep things under control.
Practical Checklist Before Starting Prednisolone
- Write down every prescription, over‑the‑counter pill, supplement, and herb you take.
- Tell your doctor about NSAIDs, warfarin, ketoconazole, clarithromycin, rifampin, ritonavir, and any live vaccines you’ve received recently.
- Ask if dose adjustments or alternative drugs are needed for your specific health conditions.
- Plan regular lab tests: blood glucose, INR (if on warfarin), and bone‑density scans for long‑term users.
- Set reminders to monitor for new symptoms-stomach pain, bruising, unusually high sugar, or mood swings.
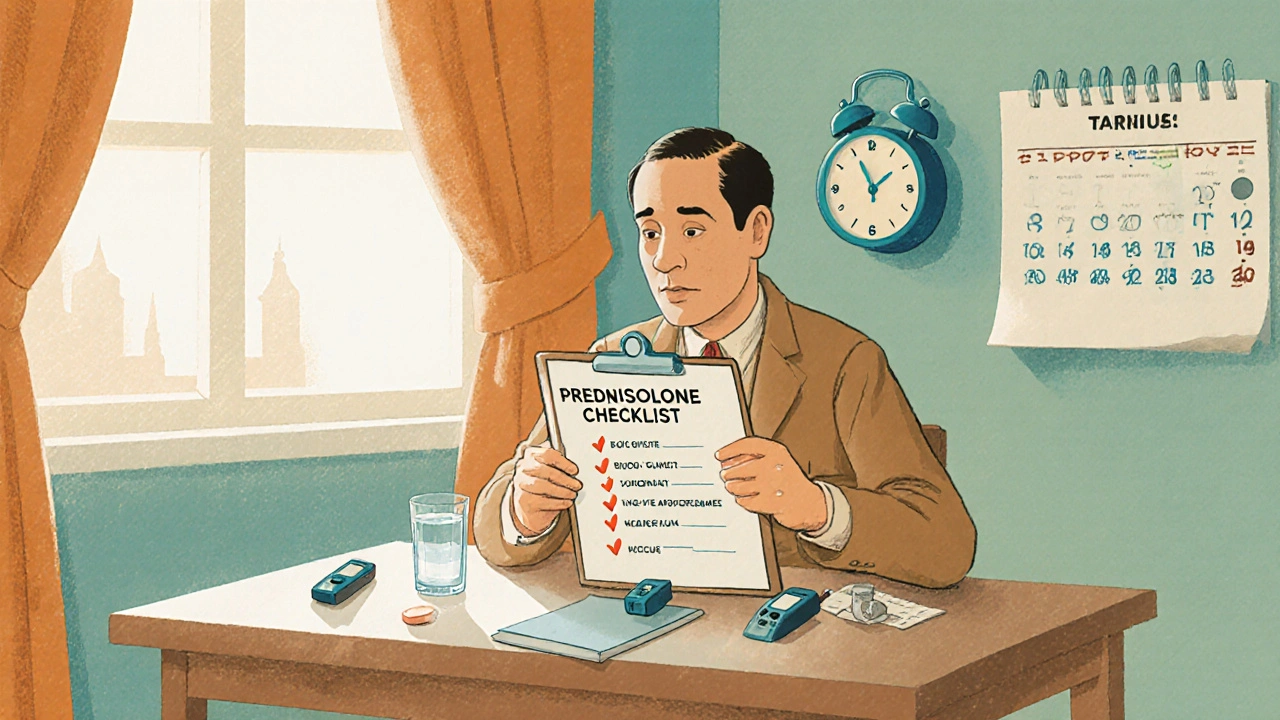
Table of Common Interacting Drugs
| Medication Class | Interaction Effect | Clinical Outcome | Recommendation |
|---|---|---|---|
| NSAIDs (ibuprofen, naproxen) | Additive GI irritation | Higher ulcer/bleeding risk | Use acetaminophen or protect with a proton‑pump inhibitor |
| Warfarin | Enhanced anticoagulant effect | INR spikes, bleeding | More frequent INR checks, possible dose reduction |
| Ketoconazole / Clarithromycin | CYP3A4 inhibition → ↑ prednisolone levels | Elevated blood pressure, glucose, mood changes | Consider alternative antifungal/antibiotic or lower steroid dose |
| Rifampin | CYP3A4 induction → ↓ prednisolone levels | Reduced anti‑inflammatory effect | Increase prednisolone dose or switch steroid |
| Ritonavir | Strong CYP3A4 inhibition | Same as ketoconazole - heightened steroid side‑effects | Close monitoring, possible dose adjustment |
| Live vaccines | Immune suppression | Vaccine may fail or cause infection | Give vaccines before starting steroids or use inactivated versions |
| Metformin & other diabetes meds | Prednisolone‑induced hyperglycaemia | Higher blood sugar, possible ketoacidosis | Temporarily increase diabetes medication dose, monitor glucose |
Frequently Asked Questions
Can I take ibuprofen with prednisolone?
It’s possible, but the combo raises ulcer and bleeding risk. If you need pain relief, ask your doctor about acetaminophen or a short‑term proton‑pump inhibitor for protection.
Why does prednisolone affect my blood sugar?
Prednisolone mimics cortisol, a hormone that tells the liver to release glucose. This can push blood‑sugar numbers up, especially for people with diabetes. Monitoring and occasional dose tweaks of your diabetes meds keep things steady.
Is it safe to get the flu shot while on prednisolone?
The flu shot is an inactivated vaccine, so it’s generally safe and still works, though the immune response may be a bit weaker. Live vaccines (like MMR) should be avoided during high‑dose courses.
What should I watch for if I’m also taking warfarin?
Check your INR more often - at least weekly when you start or change the steroid dose. Signs of excess thinning include unusual bruising, nosebleeds, or dark stools.
Do herbal supplements interact with prednisolone?
Some herbs, like St. John’s wort, induce CYP3A4 and can lower steroid levels. Others, like licorice root, may boost blood‑pressure effects. Always list supplements to your prescriber.
How long do drug‑interaction effects last after stopping prednisolone?
Prednisolone’s half‑life is about 2-4 hours, but its biological effects linger for days. Enzyme‑inducing or -inhibiting drugs may continue to affect metabolism for a week or more, so follow‑up labs are wise.

Margaret pope
October 18, 2025If you’re on prednisolone, make a list of every pill, supplement and herb you take – it really helps the doc spot risky combos.
A quick chat with your pharmacist can catch hidden interactions before they become a problem.
Karla Johnson
October 18, 2025Prednisolone is a powerhouse steroid, and when you start mixing it with other meds you’re basically walking a tightrope over a pit of bugs.
The first thing to watch is any NSAID – ibuprofen, naproxen, anything that bruises your gut – because the combo can turn a simple stomach ache into a bleeding ulcer.
Warfarin lovers, brace yourselves: prednisolone can crank up the anticoagulant effect, making your INR jump like it’s on a roller coaster, so you’ll need blood tests more often than you check your phone.
Then there are the CYP3A4 inhibitors, like ketoconazole and clarithromycin, which act like a traffic jam for the liver, letting prednisolone pile up and cause mood swings, high blood pressure, or crazy glucose spikes.
On the flip side, enzyme inducers such as rifampin and some anticonvulsants speed the drug out of your system, meaning you might feel like the steroid isn’t doing anything at all.
Ritonavir, the HIV med, is another strong inhibitor – you’ll see the same boost in steroid levels, so dose adjustments become a must.
Don’t forget about live vaccines; prednisolone can blunt the immune response, turning what should be a protective jab into a potential infection risk.
If you have diabetes, be ready for your sugar to rise; you may have to bump up metformin or whatever you’re using to keep glucose in check.
Even over-the-counter supplements matter – St. John’s wort can lower steroid levels, while licorice root can push blood pressure higher, so always tell your doctor about every herb.
The bottom line is that prednisolone touches a lot of pathways, so any drug that tweaks liver enzymes, blood clotting, or immune function can tip the balance dramatically.
When you’re prescribed prednisolone, ask for a full medication review – it’s better to spend ten minutes now than deal with a bleed or a spike later.
Regular labs are your friends: check blood sugar, INR if you’re on warfarin, and consider a bone‑density scan if you’ll be on steroids long term.
Stay vigilant for signs like stomach pain, unusual bruising, sudden mood changes, or high blood sugar – those are red flags that an interaction might be happening.
And finally, keep a written list of all your meds, supplements and vaccines; it’s the simplest tool that can prevent a cascade of complications.
Linda A
October 18, 2025In the theater of pharmacology, prednisolone takes the lead, yet the supporting cast of enzymes and co‑medications often script a tragedy unnoticed by the audience.
When CYP3A4 inhibitors step onto the stage, they whisper to the liver, "slow down," and the steroid lingers longer than intended, casting shadows of hyperglycemia and hypertension.
Conversely, inducers shout, "clear the stage!" and the steroid exits prematurely, leaving inflammation unchecked.
This delicate choreography reminds us that every pill is a character with motives, and ignoring their back‑story can turn a benign drama into a catastrophe.
Joe Moore
October 18, 2025Yo, they don’t tell you that Big Pharma loves to hide these combo dangers so you stay dependent – they push steroids while feeding you the enzyme blockers that make you need even more prescriptions.
It’s like a secret pact, and the only way out is to read the fine print and question every new drug they hand you.
Ayla Stewart
October 18, 2025Keep a running note of any over‑the‑counter meds like ibuprofen or herbal teas – even something as simple as St John’s wort can change how prednisolone works in your body.
Stephanie Zaragoza
October 18, 2025While the article does a decent job outlining major interactions, it omits the crucial point that concomitant use of high‑dose proton‑pump inhibitors can further exacerbate hypomagnesemia, especially when combined with long‑term corticosteroid therapy, and this oversight may lead clinicians to underestimate the cumulative risk of electrolyte disturbances, which in turn can precipitate cardiac arrhythmias; therefore, a comprehensive monitoring plan should include periodic serum magnesium checks in addition to the standard glucose and INR measurements, and patients should be counseled on dietary sources of magnesium to mitigate this avoidable complication.
James Mali
October 19, 2025This article feels like a copy‑paste from a drug‑info website.
Janet Morales
October 19, 2025Honestly, the piece reads like a bland textbook; you need more punch about how terrifying it is to have your blood thin to the point of bleeding just because someone slipped a NSAID in with your steroid.
Tracy O'Keeffe
October 19, 2025Well, look at you trying to sound all serious – “terrifying” is such a melodramatic choice, darling, when the real horror is how the pharma giants keep these interactions hidden behind legal jargon and fine‑print labyrinths that only lawyers can navigate.
Rajesh Singh
October 19, 2025From an ethical standpoint, clinicians have a duty to educate patients about every possible interaction, not just the headline makers; failing to do so undermines informed consent and erodes trust in the medical system.
Albert Fernàndez Chacón
October 19, 2025Totally agree – simple check‑lists and clear talk with your doctor can go a long way in keeping everything safe.
Mike Hamilton
October 19, 2025In my view, the cultural narrative around steroids often glorifies their power while downplaying the nuanced web of metabolic pathways they disturb; a broader perspective would help patients see the bigger picture.
Matthew Miller
October 19, 2025Let’s turn that awareness into action – set reminders, use apps to track meds, and share your story so others don’t slip into the same pitfalls!
Alex Lineses
October 19, 2025Great points! Leveraging medication‑management tools and fostering open communication with your care team are essential strategies to mitigate interaction risks and empower patients in their therapeutic journeys.