27 Jan 2026
- 12 Comments
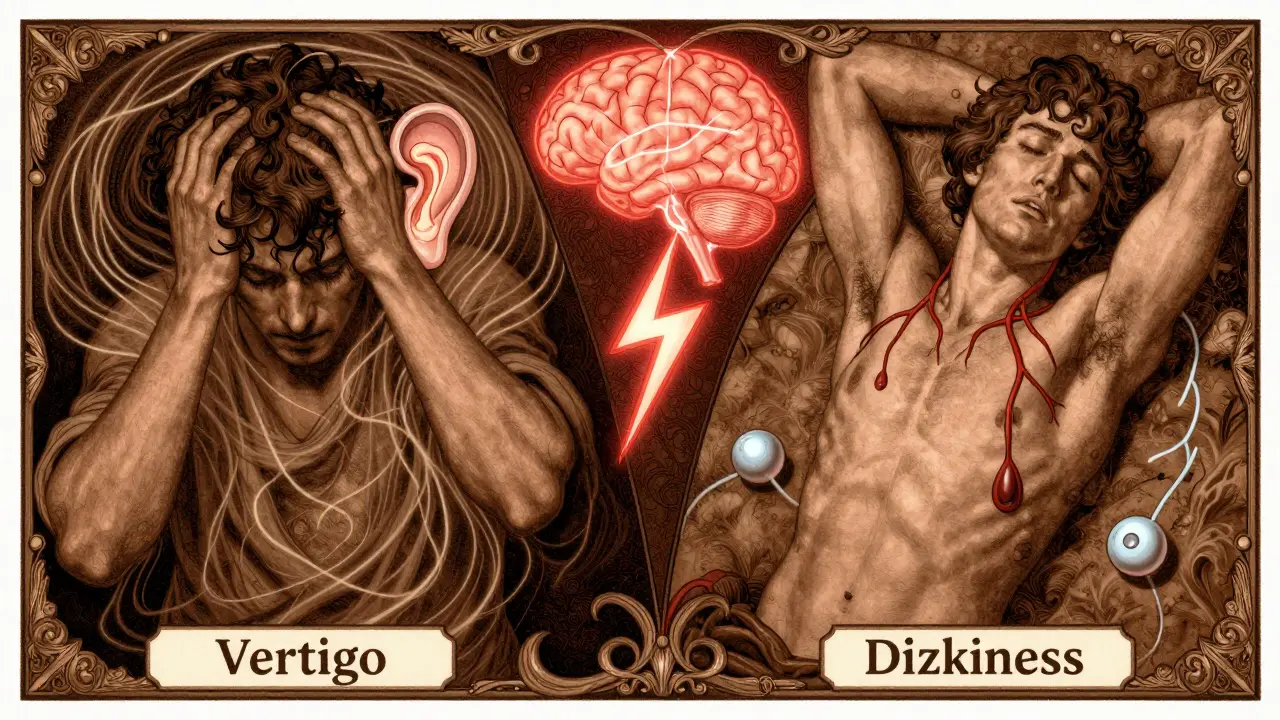
When you feel like the room is spinning, you might call it dizziness. But if you’re actually feeling like you’re on a merry-go-round even when you’re lying still, that’s not just dizziness - that’s vertigo. And confusing the two can delay real treatment by months, sometimes years.
Vertigo Isn’t Just Dizziness - It’s a Hallucination of Motion
Vertigo isn’t a feeling of being lightheaded or unsteady. It’s a false sensation of movement. You might feel like your bed is spinning, the walls are tilting, or the floor is moving beneath you - even when you’re completely still. This isn’t anxiety. It’s not stress. It’s your brain getting mixed signals from your inner ear or brainstem.
Think of your inner ear like a high-precision gyroscope. Inside each ear are three fluid-filled semicircular canals that detect head rotation, and two tiny sacs (the utricle and saccule) that sense gravity and straight-line motion. These send signals to your brain at speeds of 100-200 milliseconds. When those signals get scrambled - whether from loose crystals, inflammation, or a stroke - your brain thinks you’re moving when you’re not. That’s vertigo.
Dizziness, on the other hand, is more like feeling faint, woozy, or off-balance without any spinning. You might feel like you’re about to pass out when you stand up, or that your legs are heavy and disconnected from your body. It’s not a hallucination of motion. It’s a breakdown in your body’s ability to maintain stable balance.
What Causes Vertigo? The Big Three Vestibular Culprits
Most vertigo cases come from the inner ear - the peripheral vestibular system. Three conditions account for nearly 80% of them:
- Benign Paroxysmal Positional Vertigo (BPPV) - This is the most common cause, making up 20-30% of all vertigo cases. Tiny calcium crystals (otoconia) break loose from their normal spot in the inner ear and float into the semicircular canals. When you move your head - rolling over in bed, looking up, or bending down - those crystals shift and send false signals. Symptoms last seconds to minutes and are triggered by specific head positions. It’s harmless but terrifying.
- Vestibular Neuritis or Labyrinthitis - This is an inner ear infection, usually viral. It causes sudden, intense vertigo that can last days, often with nausea and vomiting. Unlike BPPV, it doesn’t come and go with head movement. It’s constant. The good news? Most people recover fully within weeks with rest and vestibular rehab.
- Ménière’s Disease - This involves fluid buildup in the inner ear. It causes vertigo attacks lasting 20 minutes to several hours, along with ringing in the ear (tinnitus), hearing loss, and a feeling of fullness. Attacks can be unpredictable and disabling. About 1 in 1,000 people in the U.S. have it - around 615,000 people total.
These are all peripheral causes - meaning they start in the inner ear. But vertigo can also start in the brain.
Neurological Vertigo: When the Brain Itself Is the Problem
Only 5-10% of vertigo cases are neurological, but they’re the ones that can be life-threatening. When vertigo comes from the brainstem, cerebellum, or thalamus, it’s often a sign of something more serious.
Here’s what to watch for:
- Vestibular migraine - This is the most common neurological cause of vertigo, affecting 7-10% of vertigo patients. You don’t need a headache to have it. Just five episodes of moderate-to-severe spinning, lasting 5 minutes to 72 hours, with nausea or sensitivity to light/sound, can qualify. Many people are misdiagnosed with sinusitis or anxiety.
- Stroke or TIA - A stroke in the back of the brain (posterior circulation) can cause vertigo without any limb weakness. But it’s usually accompanied by other red flags: double vision, slurred speech, trouble walking, numbness on one side, or sudden, severe headache. If you have vertigo plus any of these, get to the ER immediately.
- Multiple sclerosis - MS can attack the nerves connecting the inner ear to the brain. Vertigo may be the first symptom, often paired with blurred vision or tingling.
The key difference? Neurological vertigo rarely goes away with head movement. It’s constant. And it often comes with other neurological signs - things you wouldn’t expect from a simple ear problem.
Dizziness Has a Much Wider Range of Causes
While vertigo is mostly about the inner ear or brainstem, dizziness can come from almost anywhere in your body.
- Orthostatic hypotension - Your blood pressure drops when you stand up. A drop of 20 mmHg or more can make you feel faint. This is common in older adults, people on blood pressure meds, or after dehydration.
- Anemia or low blood sugar - When your brain doesn’t get enough oxygen or glucose, you feel lightheaded. No spinning. Just weakness and fog.
- Medication side effects - Antibiotics, antidepressants, blood pressure pills, even some allergy meds can cause dizziness. It’s not always obvious.
- Anxiety and panic disorders - Chronic dizziness is a hallmark of health anxiety or panic disorder. But here’s the catch: if you’ve had a prior vestibular injury (like a concussion), anxiety can turn into a condition called Persistent Postural-Perceptual Dizziness (PPPD), which sticks around for years.
One study found that 50% of older adults with dizziness have two or more causes - maybe low blood pressure, mild anemia, and anxiety all working together. That’s why treating just one thing often doesn’t help.
How Doctors Tell the Difference - And Why It Matters
Getting the right diagnosis changes everything. A misdiagnosed BPPV patient might take anxiety meds for a year and never get better. But the right test - a simple head movement called the Dix-Hallpike - can confirm BPPV in under a minute.
Here’s what clinicians look for:
- Nystagmus - Involuntary eye movements. In peripheral vertigo (like BPPV), the eyes jerk in one direction and then snap back. In central vertigo (brain-related), the jerking is irregular, changes direction, or happens when you look straight ahead.
- Head impulse test - The doctor quickly turns your head while you focus on a target. If your eyes dart away and then correct, your inner ear isn’t working properly.
- Videonystagmography (VNG) - This test uses special goggles to record eye movements while you follow lights or get cold/warm air in your ears. It’s 95% accurate for detecting inner ear problems.
- Red flags - New weakness, numbness, slurred speech, double vision, or loss of coordination? That’s not just dizziness. That’s a neurological emergency.
According to King Edward VII Hospital’s 2022 data, patients correctly diagnosed with BPPV had an 85% recovery rate after one Epley maneuver. Those misdiagnosed as having general dizziness? Only 45% improved - because they were treated for the wrong thing.
Treatment: What Actually Works
There’s no one-size-fits-all fix. But here’s what science says works for each type:
- BPPV - The Epley maneuver. It’s a series of head positions that guide the loose crystals back where they belong. Done correctly, it works 80-90% of the time. Many people feel better after one session. You can do it at home - but only after a professional confirms it’s BPPV.
- Vestibular neuritis - Rest for a few days, then start vestibular rehab. This is a set of exercises that train your brain to rely less on the damaged inner ear and more on your vision and body senses. It takes 6-8 weeks, but 89% of patients see major improvement.
- Ménière’s disease - Salt restriction, diuretics, and in severe cases, gentamicin injections into the middle ear to gently disable the overactive inner ear. New FDA-approved transtympanic protocols are making this safer and more effective.
- Vestibular migraine - Preventive meds like beta-blockers or antidepressants, plus migraine triggers avoidance (caffeine, chocolate, stress, lack of sleep). There’s no cure, but 70% of patients get better with the right combo.
- Orthostatic dizziness - Drink more water, avoid standing too long, wear compression socks, and rise slowly. Sometimes adjusting blood pressure meds helps.
One patient on Reddit said: “After 9 months of spinning, one Epley maneuver at the clinic - 15 minutes - and it was gone. I cried.”
Another said: “Two years of antidepressants for ‘anxiety dizziness.’ Turned out to be vestibular migraine. I finally got help after a VNG test.”
Why So Many People Get Misdiagnosed
Here’s the ugly truth: most primary care doctors aren’t trained to diagnose vertigo. A 2023 survey found only 12% of them feel “very confident” in telling BPPV apart from a stroke.
Vertigo is often mistaken for:
- Sinus infection (because of head pressure)
- Anxiety or depression (because symptoms are unpredictable)
- Old age (as if dizziness is normal - it’s not)
- Stress (when it’s actually a detached crystal in your ear)
One study found that 30% of vestibular migraine cases are initially labeled as sinusitis or anxiety. Another found that 68% of people with vertigo wait over 8 months for a correct diagnosis.
And if you have PPPD - that chronic dizziness after a concussion or inner ear injury - doctors still sometimes say, “It’s all in your head.” But it’s not. It’s a real neurological rewiring. Vestibular rehab can help. But only if you get the right referral.
What You Should Do Next
If you’ve had dizziness or vertigo for more than a few days:
- Write down your symptoms: Is it spinning? Or just lightheaded? Does it happen with head movement? Any hearing loss, ringing, or numbness?
- See a doctor who specializes in balance disorders - an ENT (otolaryngologist) or neurologist with vestibular training.
- Ask for a VNG test or head impulse test. Don’t accept a diagnosis of “anxiety” without ruling out inner ear or brain causes.
- If you have any red flags - double vision, slurred speech, weakness - go to the ER. Don’t wait.
- If you’re diagnosed with BPPV, ask for the Epley maneuver. It’s fast, free, and effective.
Vertigo and dizziness aren’t the same. One is a spinning illusion. The other is a feeling of faintness. One comes from your ear. The other from your heart, your blood, your brain, or your nerves. Getting the right diagnosis isn’t just about feeling better - it’s about catching something dangerous before it’s too late.
Is vertigo the same as dizziness?
No. Dizziness is a general term for lightheadedness, unsteadiness, or feeling faint. Vertigo is a specific type of dizziness where you feel like you or your surroundings are spinning, even when you’re still. It’s caused by a mismatch in signals from your inner ear or brain.
Can anxiety cause vertigo?
Anxiety doesn’t cause true vertigo, but it can make you feel dizzy. More importantly, if you’ve had a prior inner ear problem - like a virus or concussion - anxiety can trigger a chronic condition called Persistent Postural-Perceptual Dizziness (PPPD), where your brain becomes overly sensitive to motion. This isn’t “all in your head” - it’s a real neurological adaptation.
How do I know if my vertigo is from my ear or my brain?
Inner ear vertigo (like BPPV) usually comes with nausea, lasts seconds to minutes, and is triggered by head movements. Brain-related vertigo often comes with other symptoms: double vision, slurred speech, weakness, numbness, or trouble walking. If you have any of these, it’s a red flag for stroke or MS - get checked immediately.
Can vertigo go away on its own?
Sometimes. Vestibular neuritis often improves on its own within weeks. BPPV can resolve spontaneously, but it often comes back. Vestibular migraine and Ménière’s disease need management. The key is not waiting - early treatment with vestibular rehab or repositioning maneuvers speeds recovery and prevents long-term problems.
What’s the best test for vertigo?
The best initial test is a physical exam by a specialist - including the Dix-Hallpike maneuver for BPPV and the head impulse test for vestibular nerve damage. For more complex cases, videonystagmography (VNG) is the gold standard. It records eye movements with special goggles to detect subtle signs of inner ear or brain dysfunction.
Is vertigo dangerous?
Most vertigo isn’t dangerous - BPPV and vestibular neuritis are common and treatable. But vertigo caused by a stroke, tumor, or MS can be life-threatening. If vertigo comes with new weakness, vision changes, trouble speaking, or loss of coordination, treat it like a medical emergency. Don’t wait - go to the ER.
Can I treat BPPV at home?
Yes - but only after a doctor confirms it’s BPPV. The Epley maneuver is safe and effective when done correctly. Many online videos show how to do it. But if you have neck problems, severe arthritis, or a history of stroke, you should do it under supervision. Doing it wrong won’t hurt you, but it won’t help either.
How long does vestibular rehab take?
Most people start seeing improvement in 2-4 weeks. Full recovery usually takes 6-8 weeks of daily exercises. It’s not quick, but it’s highly effective - 89% of patients report major improvement. The exercises retrain your brain to use other senses for balance when your inner ear isn’t working perfectly.


Ambrose Curtis
January 28, 2026Man, I spent 14 months thinking I had anxiety until my ENT did the Dix-Hallpike and bam - BPPV. Those crystals were just chillin’ in my posterior canal like they owned the place. Did the Epley at home after the doc showed me, and within 48 hours? Gone. No meds. No therapy. Just gravity doing its job. Why do doctors even bother with SSRIs first?
Amber Daugs
January 30, 2026Wow. Just… wow. This is the kind of clarity I wish my primary care doctor had. Most of them treat dizziness like it’s a side effect of bad coffee or too much screen time. People are suffering for YEARS because no one takes the vestibular system seriously. This post should be mandatory reading for every med student. Seriously. Save someone’s life today.
Irebami Soyinka
January 30, 2026Y’all in the West act like vertigo is some new-age mystery. In Lagos, we call it ‘the devil’s spin’ - and we know when it’s ear or brain. If you got headache + spinning + numb fingers? Go to hospital. No waiting. No ‘maybe it’s stress.’ My cousin waited 11 months because her doctor said ‘you’re just anxious.’ She had a small stroke. Now she walks with a cane. Don’t be that person.
Brittany Fiddes
February 1, 2026Oh please. You think this is groundbreaking? I’ve been screaming about this since my 2018 vestibular migraine episode. And yet, every time I go to a GP, they hand me a prescription for Xanax and tell me to ‘try yoga.’ Like my brainstem is a mood ring. I’m not ‘anxious’ - my semicircular canals are staging a coup. If you’re not testing for nystagmus before prescribing antidepressants, you’re not a doctor. You’re a glorified pharmacist with a stethoscope.
Phil Davis
February 1, 2026Interesting. So vertigo = hallucination. That’s… actually a really elegant way to put it. Like your brain’s running a simulation it shouldn’t be. Makes you wonder how many other ‘normal’ sensations are just poorly calibrated neural noise. Maybe all perception is just a best guess with a 200ms lag. Either way - if your ears lie, your brain believes it. Scary stuff.
Linda O'neil
February 2, 2026If you’ve had dizziness for more than a week - stop Googling. Stop self-diagnosing. Go see a vestibular specialist. Not your PCP. Not an urgent care. A specialist. I was told I had ‘chronic stress’ for 3 years. Turned out I had bilateral BPPV AND vestibular neuritis. One Epley + 6 weeks of rehab = back to hiking, dancing, and not being scared to turn my head. You deserve to feel normal again. Don’t wait.
Robert Cardoso
February 4, 2026Let’s be real - the entire medical industrial complex profits from keeping people confused. Anxiety meds? Monthly prescriptions. Physical therapy? Insurance won’t cover it unless you’ve had 10 failed treatments first. Meanwhile, the Epley maneuver costs $0 and works in 15 minutes. But you can’t monetize a head tilt. So they keep you on SSRIs for 2 years. Classic capitalism. You’re not broken. You just need your crystals repositioned.
James Dwyer
February 4, 2026This gave me chills. I had vestibular neuritis after a cold in 2020. Thought I was dying. Took 6 weeks of daily rehab exercises. Now I’m stronger than ever. I even teach them to others at the community center. It’s not just about balance - it’s about reclaiming your life. You can heal. You just have to know where to look.
jonathan soba
February 5, 2026It’s amusing how Western medicine treats the inner ear like a black box. You don’t diagnose vertigo with a questionnaire and a pill. You diagnose it with physics - fluid dynamics, inertia, neurology. Yet we let generalists guess. And then we wonder why people get worse. It’s not negligence. It’s systemic incompetence. The system isn’t designed to cure. It’s designed to bill.
Chris Urdilas
February 6, 2026My mom had PPPD after a concussion. Doctors told her it was ‘psychosomatic.’ She cried every day for two years. Then she found a vestibular therapist who actually knew what she was talking about. Now she runs marathons. The brain rewires. But only if you give it the right input. Don’t let anyone tell you it’s ‘all in your head’ - your head is the problem, and it needs fixing.
SRI GUNTORO
February 7, 2026Why do Americans always need a test? In India, we just know. If your head spins when you roll over - it’s BPPV. If you feel like you’re falling and your vision blurs - it’s brain. No goggles needed. No $$$ spent. Just common sense and respect for your body. This post is over-engineered. Sometimes, the answer is simple.
Jeffrey Carroll
February 7, 2026Thank you for this meticulously detailed and clinically accurate breakdown. As someone who has spent years navigating the labyrinth of misdiagnoses, I can confirm that early vestibular assessment drastically alters outcomes. The distinction between peripheral and central etiologies is not merely academic - it is life-preserving. I urge all clinicians to prioritize vestibular screening in primary care protocols. This is medicine at its most essential.