Bioequivalence: What It Means for Generic Drugs and Your Health
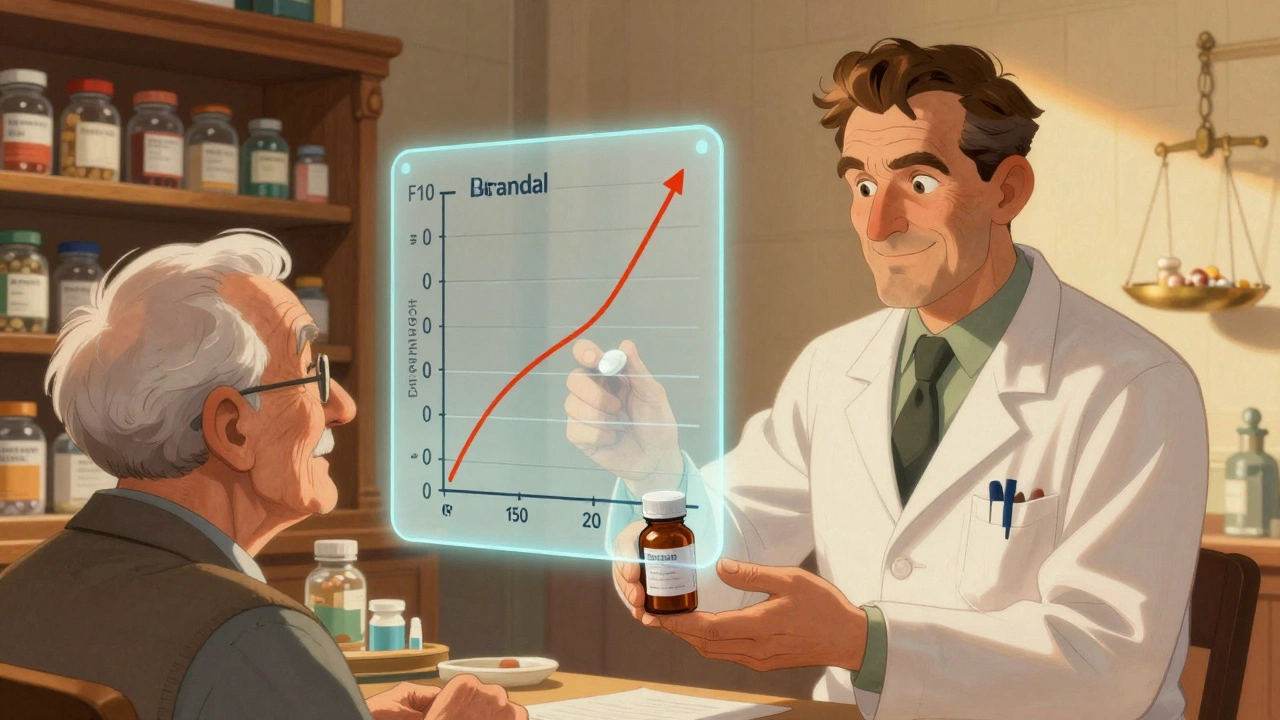
When you hear bioequivalence, the scientific standard that proves a generic drug performs the same way in the body as its brand-name version. It means the active ingredient enters your bloodstream at the same rate and amount, so your body reacts the same way—no guesswork, no risk. This isn’t marketing jargon. It’s a strict FDA requirement. If a drug doesn’t meet bioequivalence standards, it can’t be sold as a generic. That’s why your $10 pill works just like the $100 one.
What makes bioequivalence real? It’s all about drug absorption, how quickly and completely your body takes in the medicine. Two drugs are bioequivalent if their blood concentration curves match within a narrow range—usually 80% to 125%. That’s not a wide margin. It’s tight enough to ensure your blood pressure stays stable, your thyroid levels stay on track, and your antibiotics actually kill the infection. This is why switching from brand to generic doesn’t mean switching results. It means switching savings.
But bioequivalence isn’t just about the active ingredient. It also considers how the drug is made—fillers, coatings, release timing. A generic pill that dissolves too fast or too slow fails the test. That’s why some people notice differences when switching brands: not because the medicine doesn’t work, but because the formulation changed slightly. Your pharmacist can tell you if the generic you’re getting is from the same manufacturer as before.
And here’s the kicker: therapeutic equivalence, the clinical outcome that follows bioequivalence isn’t always obvious. You won’t feel a difference. You won’t see a chart. But your INR levels, your cholesterol numbers, your blood sugar—all of them stay steady because the drug did exactly what it was supposed to. That’s the power of bioequivalence. It’s the invisible guarantee behind every generic you pick up.
That’s why the posts below cover what really matters: how to spot safe generics, when to ask your pharmacist about switching, how insurance tiers affect access, and why some people still hesitate even when science says it’s fine. You’ll find real stories about people saving hundreds on statins, thyroid meds, and blood thinners—all because bioequivalence made it possible. No hype. No theory. Just what works.
Quality by Design in Generic Drug Development: Science-Based Approaches for Better Quality and Approval Rates
Quality by Design (QbD) revolutionizes generic drug development by integrating science and risk management from the start. Learn how it reduces FDA review times, cuts costs, and improves product quality. Real-world examples and future trends in this detailed guide.
Fasted vs Fed State Testing: Why Both Conditions Matter for Health and Medications
Fasted and fed state testing reveal how food impacts drug absorption and exercise performance. Understanding both conditions helps ensure medications work properly and training delivers real results.
Age and Sex in Bioequivalence Studies: What Regulators Require Today
Modern bioequivalence studies must account for age and sex differences to ensure generic drugs work safely for everyone. Learn what the FDA, EMA, and other regulators require today-and why outdated study designs are no longer enough.
Bioequivalence and Patient Safety: Why Testing Ensures Safe Generic Medications
Bioequivalence testing ensures generic drugs work as safely and effectively as brand-name versions. Learn how this science protects patients, saves billions, and keeps the healthcare system running.