31 Dec 2025
- 8 Comments
Running hurts-not the good kind of burn, but the sharp, nagging pain along your shin that won’t go away. You push through it, thinking it’s just shin splints. But what if it’s worse? What if it’s a stress fracture? The difference isn’t just semantics-it’s weeks versus months of recovery, and a 1 in 3 chance you’ll be back in the same spot if you don’t get the rehab right.
Shin Splints vs Stress Fractures: Know the Difference
Shin splints, or medial tibial stress syndrome (MTSS), feel like a dull, widespread ache along the inner edge of your shinbone. It’s common, affecting up to 20% of runners. You’ll notice it at the start of a run, it might fade as you warm up, and it usually eases with rest. It’s inflammation of the muscles, tendons, and bone tissue around your tibia-not a break.
Stress fractures are different. They’re tiny cracks in the bone itself, often in the tibia or fibula. The pain is sharp, localized, and gets worse with activity. Press on the spot-it hurts. Walk on it? Still hurts. Rest doesn’t fix it fast. You might even see swelling. A 2024 review found stress fractures are twice as common in female runners, especially those with low energy availability or irregular periods. That’s not coincidence-it’s biology.
Here’s the hard truth: 42% of runners who treat shin splints like a minor annoyance end up with a stress fracture. Why? Because they keep running. The bone doesn’t heal if you keep loading it. And once you have a stress fracture, the chance of it coming back? 19-32% if you rush back.
Phase 1: Stop Running. Start Healing.
If you suspect a stress fracture, stop running. Now. No exceptions. Even if the pain is mild. Bone doesn’t heal under load. The first phase is about protecting the injury-no running, no jumping, no high-impact stuff. For shin splints, you might only need 3-7 days of reduced activity. For stress fractures? At least 4-6 weeks of non-weight bearing.
What does that look like? Walk if it doesn’t hurt. If walking hurts, use crutches or a walking boot. That’s not weakness-it’s strategy. The goal? Pain-free walking for 7 straight days. That’s your green light to move to phase two. Skipping this? You’re gambling with your running career.
During this time, maintain fitness with low-impact work: pool running, cycling, or using an AlterG anti-gravity treadmill. Studies show runners who use AlterG recover 27 days faster than those who don’t. It lets you move like a runner without stressing the bone.
Phase 2: Rebuild Strength-Not Just Endurance
Once you can walk without pain, it’s time to rebuild. But not with miles. With strength. And not just your calves.
Start with double-leg heel raises. Stand flat, rise onto your toes, hold for 2 seconds, lower slowly. Do 3 sets of 15-20 reps, once a day. That’s it. No fancy gear. Just your body and gravity. Do this for 7-10 days. If no pain, move to step-based heel raises: stand on a step, let your heel drop below the step, then raise up. This increases the range of motion and loads the tendon differently.
Now, add hip and glute work. Weak glutes? That’s often the hidden cause. Do clamshells, side leg raises, and single-leg bridges. 3 sets of 15, every other day. Why? Because your hip controls how your leg lands. If your pelvis drops when you run, your tibia absorbs the shock-instead of your muscles and tendons. That’s how stress fractures start.
Studies show 57% of runners who skip glute training re-injure within 3 months. Don’t be one of them.
Phase 3: Return to Running-The Slow Way
Here’s where most people mess up. They think, “I’ve been pain-free for 2 days. I’m good to go.” You’re not. Bone takes 90-120 days to fully remodel. Rushing = relapse.
For low-risk stress fractures (back of the shin), follow this timeline:
- Weeks 1-2: 1 minute run, 4 minutes walk. Repeat for 20 minutes total. Twice a week.
- Week 3: 1:3 ratio. 25 minutes total.
- Week 4: 1:2 ratio. 30 minutes total.
- Week 5: 1:1 ratio. 35 minutes total.
- Week 6: 3 minutes run, 1 minute walk. 40 minutes total.
For high-risk fractures (front of shin, navicular, femoral neck)? Extend this to 8-12 weeks. No shortcuts.
And here’s the rule no one tells you: never increase your total running time by more than 10% per week. Wait-that’s outdated. A 2024 review found 68% of runners with stress fractures were hurt by following the 10% rule. Why? Because bone adapts slowly. You need to listen to your body, not a number.
Instead, use the “two weeks forward, one week back” method. Run your plan for two weeks. Then drop back to the previous week’s volume. If you feel good? Move forward. If pain creeps back? Stay where you are.
Phase 4: Build Back Power and Speed
Once you’re running 30-40 minutes continuously without pain, it’s time to rebuild power. Start with double-leg hops: 2 sets of 10-15, 2x a week. Land softly. No bouncing. Then move to single-leg hops-only when you can do double-leg pain-free for 2 weeks.
Don’t rush to sprints or hills. Your bone needs time to adapt to impact. Add one speed session every 10-14 days. Start with 4 x 20-second strides on flat ground. Rest 90 seconds between. That’s it. No intervals. No long sprints. Just controlled, smooth acceleration.
Track your pain. Use a 0-10 scale. If pain hits 2 or above during or after running, stop. Back off. This isn’t weakness. It’s smart. Studies show runners who monitor pain daily have 34% fewer recurrences.
Why Most People Fail (And How to Avoid It)
Here’s what goes wrong:
- Skipping hip strength work
- Going too fast after a few pain-free days
- Ignoring nutrition
- Not sleeping enough
That last one? Huge. Bone rebuilds while you sleep. If you’re not getting 7-8 hours, you’re sabotaging your recovery. And nutrition? 31% of female runners with recurring stress fractures have undiagnosed RED-S-Relative Energy Deficiency in Sport. That means not eating enough to support training. Low calories = weak bones. No matter how much you stretch or foam roll.
Get your vitamin D and calcium checked. If you’re a woman with irregular periods, get your hormones tested. Bone health isn’t just about loading-it’s about fuel.
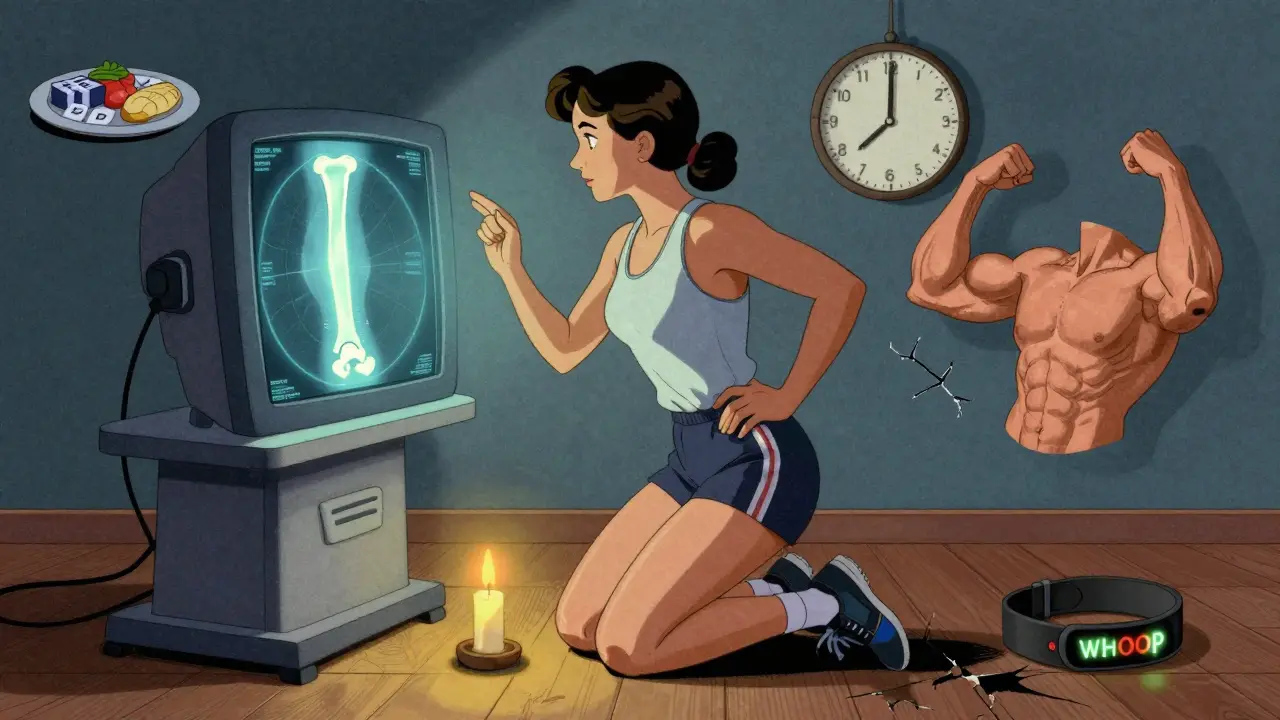
Tools That Help
Technology is making recovery smarter. The WHOOP strap now tracks bone strain with 89% accuracy. If your strain score spikes after a run, it’s a warning. The RunRx app uses AI to predict your recovery time based on your training history, sleep, and even blood markers. It’s not magic-it’s data.
And yes, physical therapy matters. Runners who work with a PT return to pre-injury mileage 22 days faster than those who go it alone. If you can’t see a PT, find a certified running coach who understands rehab. Not just someone who tells you to “run through it.”
When to See a Doctor
See a sports medicine specialist if:
- Pain lasts more than 2 weeks despite rest
- It’s sharp and localized
- You have swelling or bruising
- You’re a woman with missed periods or low energy
- You’ve had this injury before
Get an MRI. X-rays often miss early stress fractures. An MRI shows bone swelling before a crack forms. That’s your early warning.
Final Thought: Patience Isn’t Optional
You don’t lose fitness by resting. You lose it by re-injuring. A 6-week rehab plan might feel slow. But coming back too soon? That’s a 12-week setback. The best runners aren’t the fastest. They’re the ones who know when to slow down.
Heal right. Train smart. Run longer.
Can I still exercise while recovering from shin splints or a stress fracture?
Yes-but not running. Focus on low-impact activities like swimming, pool running, cycling, or using an anti-gravity treadmill. These keep your heart strong without stressing the injured bone. Avoid anything that causes pain above a 2/10 on your pain scale.
How long does it take to return to running after a stress fracture?
It depends on the location and severity. Low-risk stress fractures (like the back of the shin) usually take 6 weeks. High-risk ones (front of shin, foot bones, femur) take 8-12 weeks. Always wait until you can walk pain-free for 7 days before starting the run-walk protocol.
Is the 10% weekly mileage rule safe for returning from a stress fracture?
No. Recent studies show 68% of runners with stress fractures were injured by following the 10% rule. Bone remodeling takes 90-120 days. A fixed percentage ignores individual healing rates. Use a pain-guided, phased approach instead.
Do I need an MRI to diagnose a stress fracture?
If your pain is sharp, localized, and doesn’t improve after 2 weeks of rest, yes. X-rays often miss early stress fractures. An MRI shows bone swelling before a crack forms, giving you an earlier diagnosis and better chance to heal properly.
Why do women get stress fractures more often than men?
Women are more likely to have low energy availability, irregular periods, or low bone density-often due to Relative Energy Deficiency in Sport (RED-S). This weakens bones. It’s not just about training harder-it’s about fueling enough. All female athletes with stress fractures should be screened for RED-S.
Can I prevent shin splints and stress fractures from coming back?
Yes. Strengthen your glutes and calves, avoid sudden increases in mileage, get enough sleep and calories, and listen to your body. Use a pain scale (0-10) to guide your return. If pain hits 2 or above, stop. Recurrence drops by 34% when you rest at least one day between runs.
Should I use orthotics or heel lifts for shin splints?
Heel lifts only reduce tibial strain by 12-15%. Gait retraining-changing how you land-reduces it by 38%. Orthotics might help temporarily, but they don’t fix the root cause. Focus on strength, form, and load management instead.


LIZETH DE PACHECO
January 2, 2026I was told to run through shin pain for years until I got a stress fracture. Took me 10 weeks to get back to running and I didn’t even know about glute weakness until PT showed me. Now I do clamshells before every run like it’s prayer. No more injuries. Seriously, if you’re a woman with irregular periods and this happened to you? Get your hormones checked. It’s not weakness, it’s biology.
Lee M
January 2, 2026You call this evidence-based? You’re just repackaging orthopedic dogma as science. Bone doesn’t heal without load. You’re telling people to sit on their asses for 6 weeks like it’s a spa retreat. Adaptation happens under stress, not avoidance. This is why runners are getting weaker - because we’ve turned recovery into a religion of fear.
Matthew Hekmatniaz
January 4, 2026I’ve been through this twice. First time I listened to the ‘rest for 6 weeks’ advice and came back too fast - ended up with a navicular stress fracture. Second time? I did the full protocol: walk pain-free for 10 days, then heel raises for 3 weeks, then the run-walk plan with the two-forward-one-back rhythm. Took 14 weeks total but I’ve been injury-free for 18 months now. The glute work? Game changer. Also, sleep isn’t optional. If you’re burning the candle at both ends, your bones know.
Dusty Weeks
January 4, 2026bro i had shin splints for 8 months and just kept running lmao finally went to a doc and they were like ‘dude you have a fracture’ i was like ‘wait what?’ now i use whoop and i check my bone strain score like its my daily horoscope 🤡🩹
Paul Ong
January 6, 2026Stop running if it hurts. That’s it. No fluff. No 10% rules. No apps. Just listen. If your shin screams, you stop. Walk if you can. Bike if you want. Come back slow. No ego. No rush. The finish line isn’t tomorrow. It’s next year when you’re still running.
Austin Mac-Anabraba
January 7, 2026Let’s be clear: this article is dangerously misleading. You claim the 10% rule is obsolete, yet you provide a rigid, linear progression that is just as inflexible. You ignore individual variability in bone density, training history, and metabolic health. You cite a 2024 review but don’t link it. You blame female runners’ biology without addressing systemic issues like lack of access to sports nutritionists. This isn’t evidence-based - it’s performative medicine dressed in data.
Phoebe McKenzie
January 7, 2026OF COURSE women get stress fractures more often. You’re out here running marathons on 1200 calories a day while your body is screaming for food. You think foam rolling fixes RED-S? You think stretching heals a cracked tibia? Wake up. If you’re a woman with missed periods and you’re still running? You’re not a warrior. You’re a walking osteoporosis case. Get. Help. Now.
gerard najera
January 7, 2026Heal slow. Run longer.