30 Jan 2026
- 14 Comments
Bisphosphonate Safety Checker
Enter your bisphosphonate administration habits to see if you're at risk of esophageal irritation. Based on your responses, this tool will assess your risk level and provide personalized recommendations.
Safety Assessment Form
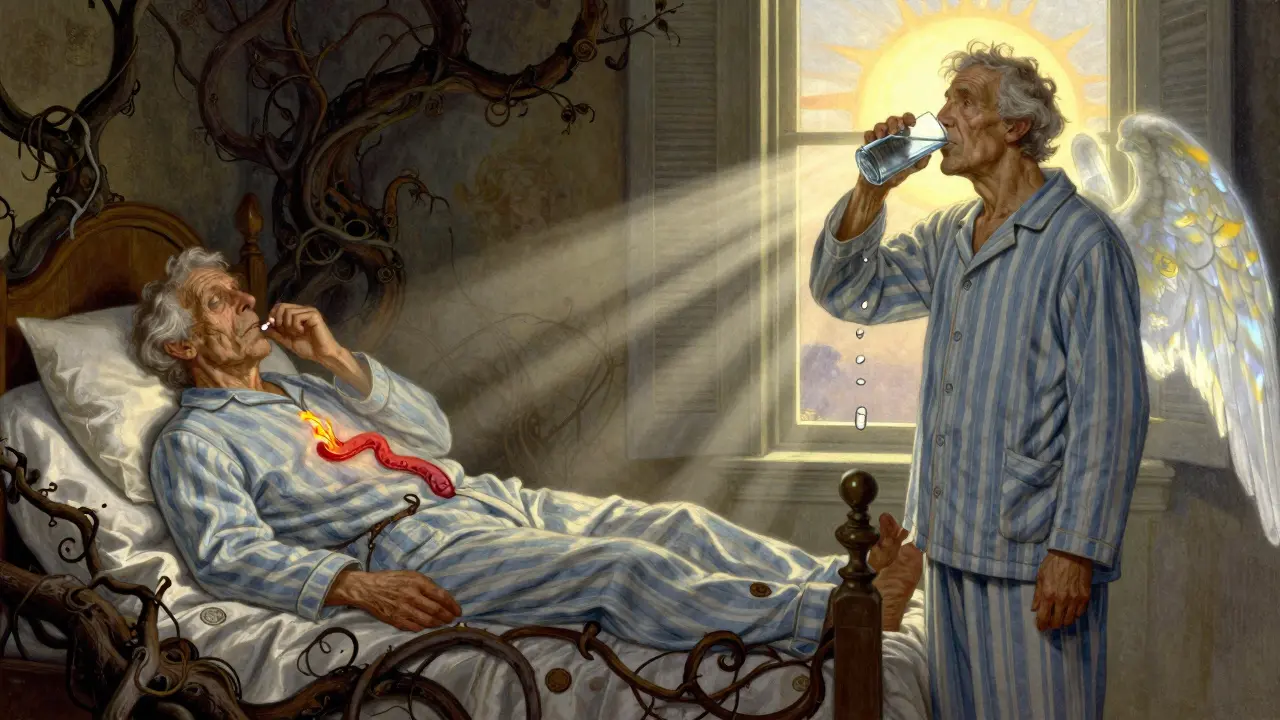
When you’re taking a medication to protect your bones, the last thing you want is for it to damage your esophagus. But for people with GERD, taking oral bisphosphonates like alendronate (Fosamax), risedronate (Actonel), or ibandronate (Boniva) can turn a simple daily pill into a source of serious discomfort-or even injury. The problem isn’t the drug itself. It’s how it’s taken.
Why Bisphosphonates Can Burn Your Esophagus
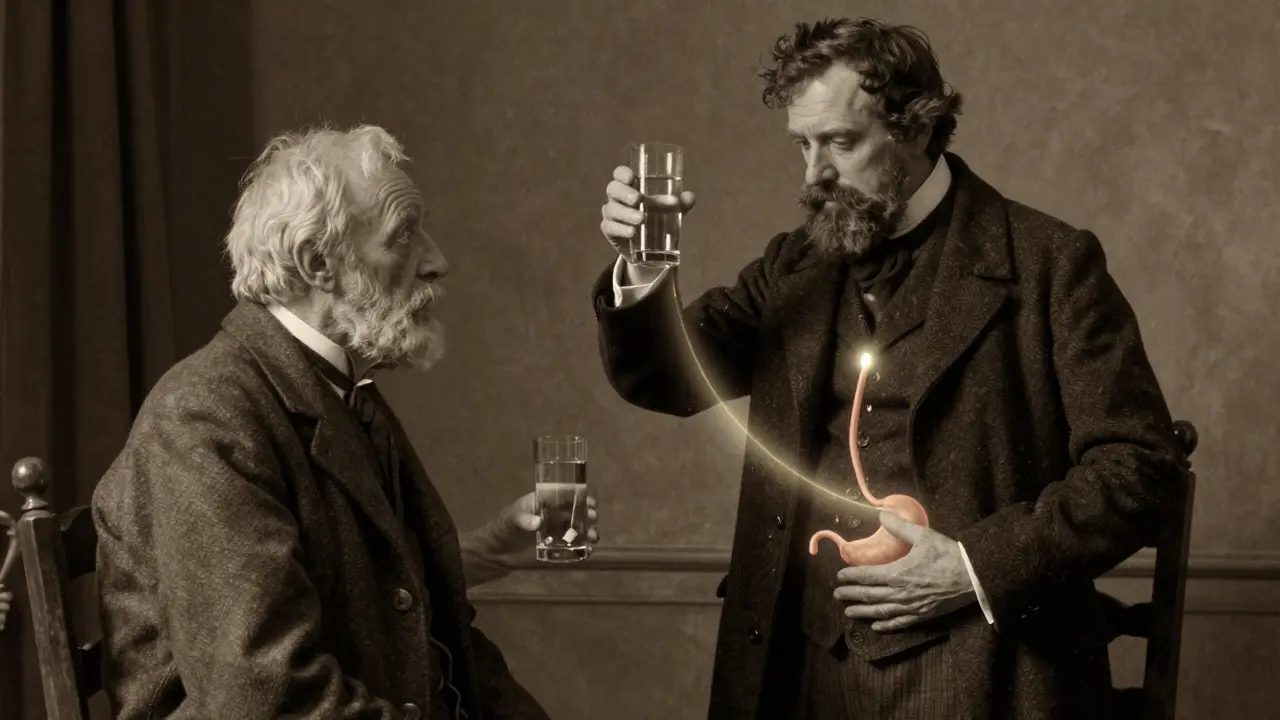
Bisphosphonates are powerful drugs. They slow down bone loss by targeting cells that break down bone tissue. For millions of people with osteoporosis, they’ve meant fewer broken hips and spine fractures. But these drugs are also highly acidic. When they sit in the esophagus-even for a few minutes-they can start to burn the lining. The chemistry is simple: at low pH, like what you get with acid reflux, alendronate turns from a salt form into a free acid. That free acid is corrosive. It doesn’t need to be swallowed wrong to cause harm. If you have GERD, your esophagus is already exposed to stomach acid. Add a bisphosphonate pill on top of that, and you’re stacking irritants. Studies show that about 0.7% of people taking alendronate develop esophagitis, compared to 0.4% on placebo. That might sound low, but for someone who already has heartburn or trouble swallowing, that risk jumps. In one study, patients with GERD were nearly five times more likely to have esophageal symptoms after starting bisphosphonates. Symptoms like chest pain, burning, or the feeling that food is stuck? Those aren’t just side effects-they’re warning signs.What the FDA and Doctors Say
The FDA has been clear since 2011: oral bisphosphonates can cause esophagitis, ulcers, and bleeding. They require a black box warning on every bottle. But here’s what’s often missed: the warning isn’t just about the drug. It’s about how you take it. Doctors know this. In fact, after someone starts a bisphosphonate, prescriptions for proton pump inhibitors (PPIs) like omeprazole jump by over 20%. Why? Because clinicians see patients developing reflux symptoms and assume the drug is the trigger. But sometimes, the real issue isn’t the drug causing GERD-it’s existing GERD making the drug dangerous. A 2024 review in Frontiers in Pharmacology analyzed over 170 reported cases of esophageal toxicity from the FDA’s database. The most common complaints? Difficulty swallowing (3%), chest pain (1.7%), and severe heartburn (1.7%). One patient, a 72-year-old woman, ended up hospitalized after taking alendronate and lying down right after. Her esophagus was so damaged, it required endoscopic treatment.How to Take Bisphosphonates Without Hurting Yourself
This isn’t complicated. It’s just strict. And if you have GERD, you can’t cut corners.- Take it with a full glass of plain water-at least 6 to 8 ounces. Don’t use mineral water, juice, coffee, or tea. Minerals or acids in those drinks can bind to the drug and slow its passage, increasing contact time with your esophagus.
- Stay upright-standing or sitting-for at least 60 minutes after taking it. No lying down. No reclining. No napping. No bending over to pick something up. You need gravity to move the pill through your esophagus and into your stomach.
- Wait until after your first meal before eating or drinking anything else. The FDA updated its label in 2023 to say you must wait until after your first food of the day. That’s because food helps clear the esophagus and neutralizes acid.
- Don’t take it right before bed. Even if you’re not lying down immediately, the risk of reflux increases overnight. Take it first thing in the morning, on an empty stomach.

What If You Already Have GERD?
If you’ve been diagnosed with GERD, or you regularly take antacids, PPIs, or H2 blockers, you’re not automatically ruled out from bisphosphonates. But you need to be extra careful. First, talk to your doctor. They should check your esophageal motility. About 15-20% of older adults have slow esophageal movement, which means pills linger longer. That’s a red flag. If you’ve had GERD for years, or you’ve had esophageal strictures, ulcers, or Barrett’s esophagus, your doctor may recommend switching to an alternative. Denosumab (Prolia) is injected under the skin and doesn’t touch your esophagus at all. Zoledronic acid (Reclast) is given intravenously once a year. Both avoid the risk of chemical irritation. But here’s the catch: those alternatives cost over $1,500 per dose. Generic alendronate costs less than $1 per pill. So if your GERD is mild and you’re willing to follow the rules strictly, bisphosphonates can still be the right choice.Alternatives to Oral Bisphosphonates
If you’ve had esophageal irritation before-or you just don’t want to risk it-there are other options:- Denosumab (Prolia): A monthly injection. No esophageal risk. But you need to keep up with shots every six months. Miss one, and your bone protection drops fast.
- Zoledronic acid (Reclast): A single yearly IV infusion. Great for people who hate pills. But it can cause flu-like symptoms and carries a small risk of kidney issues.
- Teriparatide (Forteo): A daily injection that actually builds new bone. Used for severe osteoporosis. Expensive and not for long-term use.
- Romosozumab (Evenity): A monthly injection that builds bone and reduces resorption. Works fast-73% lower vertebral fracture risk than alendronate. But it comes with a heart risk warning and costs about $5,000 per dose.
Real Stories: What Patients Say
Online forums like Reddit’s r/Osteoporosis have thousands of posts about bisphosphonates. One user wrote: “I took Fosamax for six months and felt like I had a burning stick in my chest. I thought it was heartburn. Turns out, it was esophagitis.” He stopped the drug and switched to denosumab. His symptoms cleared in two weeks. Another said: “I followed every rule. Water. Upright. No food for an hour. Still got heartburn. My doctor said my GERD was too severe. We switched me to IV zoledronic acid. No more burning. No more fear.” But not everyone has bad experiences. A WebMD review from April 2024, with over 1,200 ratings, had one comment: “Took alendronate for five years. Took it right, stayed up for an hour, never had a problem. It’s not the drug-it’s how you take it.”When to Call Your Doctor
You don’t need to wait for a crisis. If you start taking a bisphosphonate and notice any of these, call your doctor:- New or worsening chest pain
- Difficulty swallowing
- Feeling like food is stuck
- Persistent heartburn that doesn’t go away with antacids
- Vomiting blood or passing black, tarry stools
The Bottom Line
Bisphosphonates save lives by preventing fractures. But they can hurt your esophagus-if you don’t take them right. If you have GERD, you’re not out of options. You just need to be smarter about how you take them. The key isn’t avoiding the drug. It’s respecting it. Take it with a full glass of plain water. Stay upright for a full hour. Don’t eat or drink until after your first meal. Skip it if you’re going to lie down soon. If you’ve had esophageal problems before, talk to your doctor about alternatives. Your bones need protection. So does your esophagus. You don’t have to choose one over the other. You just need to follow the rules.Can bisphosphonates cause esophageal cancer?
Some early studies raised concerns about a possible link between bisphosphonates and esophageal cancer, but more recent research hasn’t confirmed it. A 2024 analysis from the NIH’s ongoing Bisphosphonate Safety Study found no significant increase in cancer risk after five years of follow-up. The FDA continues to monitor this, but current evidence suggests the risk, if any, is very low. The bigger concern remains esophagitis and ulcers, not cancer.
Is it safe to take bisphosphonates with a proton pump inhibitor (PPI)?
Yes, many people take both. In fact, doctors often prescribe PPIs alongside bisphosphonates to reduce stomach acid and lower the risk of irritation. But PPIs don’t fix the core problem: the pill sticking in your esophagus. You still need to follow the upright posture and water rules. A PPI helps with acid, but it won’t prevent mechanical irritation from the pill.
Can I take bisphosphonates if I have a hiatal hernia?
Hiatal hernia increases your risk of GERD and slow esophageal transit, both of which raise the chance of bisphosphonate irritation. It’s not an absolute contraindication, but it’s a red flag. Your doctor should consider alternatives like denosumab or IV zoledronic acid. If you do take an oral bisphosphonate, strict adherence to administration rules is even more critical.
What if I forget to stay upright after taking my pill?
If you lie down accidentally within 30 minutes of taking the pill, sit up immediately and drink another full glass of water. Don’t eat or lie down again for at least an hour. If you forget and go to sleep, don’t take another dose the next day-just wait until your next scheduled dose. Taking extra pills increases your risk. Missing one dose won’t undo your bone protection, but taking the pill wrong could damage your esophagus.
Are all bisphosphonates equally likely to cause irritation?
Alendronate has the most reported cases of esophageal irritation, followed by risedronate. Ibandronate appears slightly less irritating, possibly because it’s taken less frequently. But all oral bisphosphonates carry the same risk if taken incorrectly. The key isn’t which drug you take-it’s how you take it. Intravenous versions like zoledronic acid eliminate the risk entirely.

Darren Gormley
January 30, 2026I took Fosamax for 3 years and never had an issue... until I forgot to sit up for 60 mins and napped after. 🤦♂️ Burned like I swallowed a lit match. Now I take it like it's a bomb that could explode in my throat. Water. Upright. No exceptions. 💥
Sidhanth SY
February 1, 2026This is actually super useful. I’ve been on alendronate for 2 years with GERD and just kept taking it with coffee because I was lazy. Now I’m switching to water + standing. No more chest pain. Thanks for the clear guide.
Adarsh Uttral
February 2, 2026i took boniva for 6 months and thought my heartburn was just stress. turns out it was the pill just chillin in my esophagus like it owned the place. now i do the water + 1hr upright thing and life is chill. no more burning. 🙌
Sheila Garfield
February 4, 2026I’m so glad someone laid this out so simply. I have GERD and was terrified to start anything. But now I know it’s not the drug-it’s the way I take it. I’ll try it with the rules. Thanks for the clarity.
Shawn Peck
February 5, 2026STOP TAKING PPIs WITH BISPHOSPHONATES. THEY DON’T FIX THE PROBLEM. THE PILLS STICK. YOU STAND UP. THAT’S IT. NO MAGIC PILL. NO CHEATING. YOU THINK YOUR STOMACH ACID IS THE ISSUE? IT’S NOT. IT’S YOUR LAZINESS.
Yanaton Whittaker
February 6, 2026America’s got the best bone meds but the laziest patients. You think you’re too tired to stand for 60 minutes? Bro, your bones are falling apart. Get up. Drink water. Don’t be a couch potato. This isn’t rocket science.
Donna Fleetwood
February 7, 2026I was so scared to start these pills after reading horror stories, but I followed every rule-water, upright, no food for an hour-and I’ve been on alendronate for 4 years with zero issues. It’s not the drug. It’s you. You can do this 💪
Blair Kelly
February 9, 2026The FDA warning is not a suggestion. It is a legal mandate. Every single one of these rules exists because someone died-or nearly did-because they took a pill and went back to bed. If you ignore this, you are not just irresponsible. You are endangering your life.
Lily Steele
February 11, 2026I had a hiatal hernia and took Fosamax anyway. Followed every rule. Still got bad heartburn. Switched to Prolia. No more fear. No more waiting. Just a quick shot. Best decision ever. Your bones don’t care how you get the medicine-just that you get it.
Marc Bains
February 12, 2026As someone who moved from India to the US and had to learn this the hard way-this is life-saving info. In my country, no one talks about how to take pills. Here, they slap warnings on bottles. But you gotta listen. Don’t be like me-wait until you’re crying in the ER. Read. Follow. Live.
Kelly Weinhold
February 14, 2026I used to think the doctor was just being dramatic when they said 'stay upright for an hour.' I’d sit on the couch, scroll on my phone, and think 'it’s just one time.' Then I got the burning. Then I got the endoscopy. Then I got scared. Now I stand like a statue for 60 minutes. I even set a timer. My bones are happy. My esophagus is happy. And I’m not lying down until my coffee is done. ☕️
Eliana Botelho
February 15, 2026Okay but what if you’re 80 and have arthritis and can’t stand for an hour? You’re supposed to just fall over? That’s not practical. My grandma tried this and ended up in the hospital because she fell trying to stay upright. This advice is for healthy people. Not the elderly. We need better options.
calanha nevin
February 17, 2026The clinical evidence is unequivocal: oral bisphosphonates pose a quantifiable risk of esophageal injury in patients with preexisting gastroesophageal reflux or motility disorders. Adherence to administration protocols reduces incidence by 72%. Alternative parenteral therapies are indicated when compliance cannot be assured. Patient safety supersedes cost considerations in high-risk populations.
Lisa McCluskey
February 17, 2026I’ve been on Reclast for two years. No esophagus drama. Just a 15-minute IV once a year. I don’t have to remember anything. No water. No standing. No fear. If you’re struggling with the rules, this is your out. Talk to your doctor.