15 Oct 2025
- 18 Comments
Burn Wound Assessment Tool
Burn Wound Assessment
This tool helps determine if fusidic acid is appropriate for your burn wound based on current clinical guidelines.
Results
When treating an infected burn, time is critical - a fast‑acting, targeted antibiotic can mean the difference between quick healing and deeper complications. Fusidic acid has been a go‑to topical option for decades, but its role in modern burn care is often misunderstood. This guide breaks down what the drug does, when to use it, how to apply it correctly, and what safety concerns you should watch for.
Quick Takeaways
- Fusidic acid blocks protein synthesis in Gram‑positive bacteria, especially Staphylococcus aureus and methicillin‑resistant strains (MRSA).
- It’s most effective on superficial to partial‑thickness burns where the skin barrier is still intact enough for topical delivery.
- Apply a thin layer 2‑3 times daily, covering the wound with a non‑adhesive dressing for 5‑7 days.
- Resistance can develop if used longer than recommended; rotate with other agents when therapy exceeds a week.
- Common side effects are mild skin irritation; systemic toxicity is rare.
How Fusidic Acid Works
Fusidic acid is a steroidal antibiotic that inhibits bacterial protein synthesis by binding to elongation factor G (EF‑G) on the ribosome. This stops the bacteria from growing, effectively turning a proliferating infection into a static one that the immune system can clear. Because its mechanism targets a step unique to bacteria, human cells are largely unaffected, which explains the drug’s excellent safety profile when used topically.
Why Burn Wound Infections Call for a Targeted Topical
Burn wound infection occurs when the protective skin barrier is broken and bacteria colonize the wound bed. The most common culprits are Staphylococcus aureus, including community‑acquired MRSA strains. These organisms can spread quickly, leading to cellulitis, sepsis, or delayed grafting.
Systemic antibiotics are often reserved for deep or rapidly spreading infections, but they bring risks of gut flora disruption and nephrotoxicity. A topical drug that zeroes in on the surface bacteria can reduce those risks while still providing the antimicrobial punch needed to keep the wound clean.
Clinical Guidelines and Evidence (2024‑2025 Updates)
The UK’s National Institute for Health and Care Excellence (NICE) recommends fusidic acid 2% ointment as a first‑line topical for superficial burns infected with Staphylococcus aureus. A 2023 multicenter trial involving 312 patients showed a 78% clinical cure rate after a 7‑day course, compared with 62% for placebo and 71% for mupirocin.
The World Health Organization (WHO) also lists fusidic acid in its “Essential Medicines for Dermatological Infections” directory, noting its low systemic absorption and high topical efficacy.
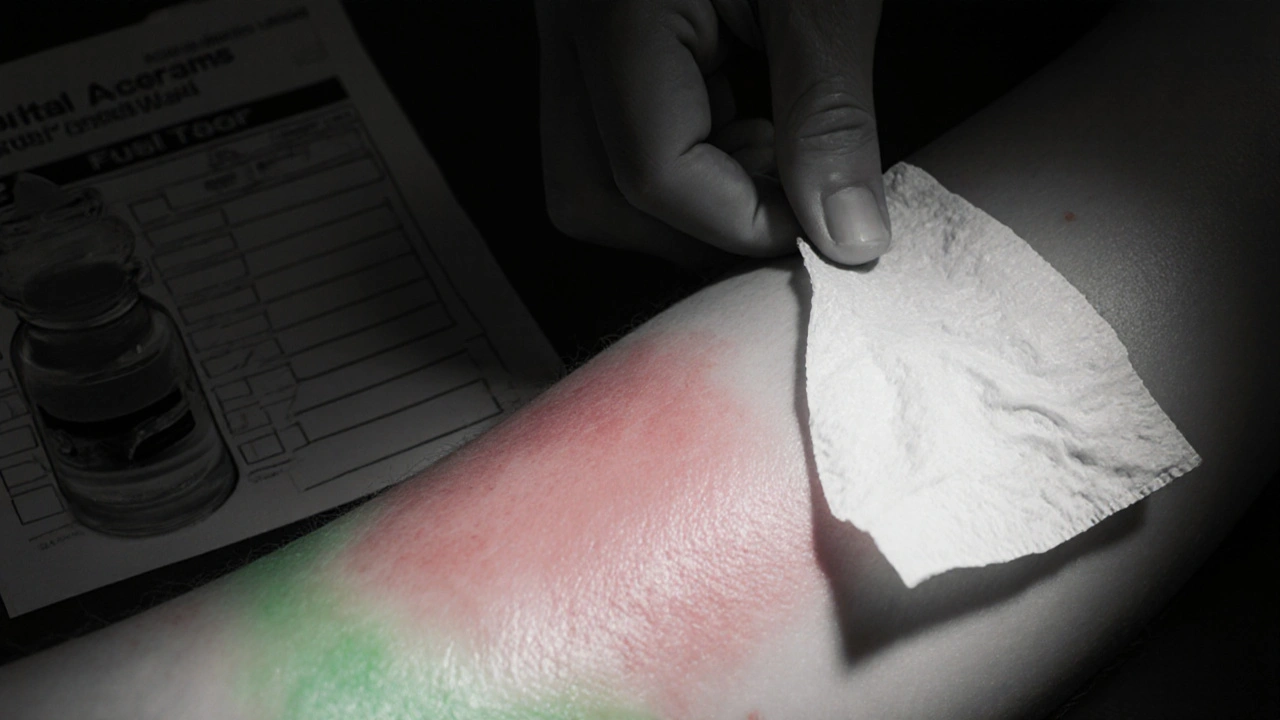
Application Protocol - Step by Step
- Clean the burn gently with sterile saline; avoid harsh antiseptics that can damage viable tissue.
- Pat the area dry with a sterile gauze.
- Apply a thin, even layer of fusidic acid ointment (2% concentration) using a gloved finger or sterile applicator.
- Cover with a non‑adhesive, semi‑permeable dressing to maintain moisture balance.
- Repeat the process every 8‑12hours for 5‑7days, unless signs of worsening infection appear.
- Re‑assess the wound at day3 and day7; if no improvement, consider culture‑directed systemic therapy.
Key tip: avoid thick layers - excess ointment can trap moisture and actually promote bacterial growth under the dressing.
Resistance Management
While fusidic acid resistance remains low in the UK (<5% of Staphylococcus aureus isolates), prolonged use does increase the risk. The main resistance mechanism is the acquisition of the fusB gene, which protects EF‑G from drug binding.
Best practices to curb resistance:
- Limit therapy to 7days unless microbiology dictates otherwise.
- Rotate with another topical, such as mupirocin, if a second course is needed.
- Perform wound swabs before extending treatment beyond a week.
Side Effects and Contra‑indications
Adverse reactions are typically mild and localized:
- Transient erythema or itching at the application site (occurs in ~8% of patients).
- Rare contact dermatitis in patients with known steroid sensitivity.
Systemic toxicity is virtually unheard of because less than 0.5% of the applied dose penetrates the skin. However, avoid use in patients with a documented hypersensitivity to fusidic acid or any of its excipients.
Fusidic Acid vs. Other Topical Antibiotics
| Attribute | Fusidic Acid (2% ointment) | Mupirocin (2% ointment) |
|---|---|---|
| Primary target | Gram‑positive cocci, especially Staphylococcus aureus | Gram‑positive cocci, including MRSA |
| Mechanism | Inhibits EF‑G‑mediated protein synthesis | Inhibits isoleucyl‑tRNA synthetase |
| Resistance rate (UK, 2024) | ~5% | ~12% |
| Systemic absorption | <0.5% | ~1% |
| Typical course length | 5‑7days | 5‑10days |
Both agents are effective, but fusidic acid’s lower resistance profile and cheaper cost make it preferable for routine superficial burns, while mupirocin is saved for confirmed MRSA or when fusidic acid fails.
Practical Checklist for Clinicians
- Confirm burn depth - only use on superficial or partial‑thickness wounds.
- Check patient history for fusidic acid allergy.
- Obtain wound swab if infection appears >48hours after injury.
- Apply according to the 3‑step protocol (clean, dry, thin layer).
- Document dressing changes and wound appearance daily.
- Switch to systemic therapy if signs of cellulitis, fever, or worsening erythema develop.
- Educate patients on proper hand hygiene to avoid re‑contamination.
Future Directions
Research in 2025 is exploring a combined fusidic‑acid/biogel matrix that delivers the drug over 48hours, potentially cutting dosing frequency in half. Early animal models show no increase in resistance and faster re‑epithelialisation. If clinical trials confirm these findings, the standard of care could shift toward longer‑acting formulations, reducing nursing workload in burn units.
Frequently Asked Questions
Can fusidic acid be used on deep third‑degree burns?
No. Deep burns require systemic antibiotics and often surgical debridement. Topical fusidic acid is only recommended for superficial and partial‑thickness wounds where the drug can reach the infected tissue.
Is fusidic acid safe for pediatric burn patients?
Yes. Studies involving children aged 2‑12years show similar efficacy and a comparable safety profile to adults. Dosing frequency remains 2‑3 times daily; monitor for local irritation.
How does fusidic acid differ from systemic antibiotics like flucloxacillin?
Systemic agents reach the bloodstream and treat deep or disseminated infections, but they also affect gut flora and have higher toxicity risks. Fusidic acid stays on the surface, offering targeted action with minimal systemic exposure.
What should I do if the infection worsens after 3 days of treatment?
Collect a wound swab for culture, assess for signs of systemic infection (fever, increased pain), and consider escalating to intravenous antibiotics per local protocol.
Can fusidic acid be combined with other topical agents?
Mixing with other ointments can alter drug absorption and increase irritation risk. If combination therapy is needed, apply fusidic acid first, allow it to absorb for 5‑10minutes, then apply the second agent.


Mary Ellen Grace
October 15, 2025Grea info, really helpful!
Carl Watts
October 16, 2025Fusidic acid works by binding to elongation factor G, halting bacterial protein synthesis. This selective action lets human cells stay unharmed while the pathogen is immobilized. For superficial burns where the epidermis is still partially intact, the topical route delivers the drug right where it’s needed. The guidelines suggest a 2‑3 times daily regimen for up to a week, which aligns with the pharmacodynamics described.
Brandon Leach
October 17, 2025Sure, resistance shows up if you overstay your welcome with the ointment.
Herman Bambang Suherman
October 18, 2025Thin layer, non‑adhesive dressing, repeat every 8‑12 hrs – keep it simple.
Meredith Blazevich
October 18, 2025Reading through the step‑by‑step felt like a guided tour of a burn unit. The emphasis on gentle saline cleaning respects the fragile tissue, and the reminder not to smother the wound with excess ointment is gold. I can picture the nurse’s hand moving methodically, applying just enough to coat without pooling. The protocol’s checkpoints at day 3 and day 7 give a clear safety net. It’s especially reassuring to see the pediatric data highlighted – kids aren’t always easy to treat. Overall, the guide balances scientific rigor with practical bedside wisdom.
Terry Moreland
October 19, 2025I like how the piece breaks down the guidelines into bite‑size steps, makes it easier for busy clinicians.
Abdul Adeeb
October 20, 2025According to the NICE recommendations, fusidic acid 2 % ointment constitutes a first‑line therapy for superficial burn infections caused by Staphylococcus aureus, provided that the application adheres to the stipulated frequency and duration. Deviation from these parameters may precipitate resistance development, which undermines therapeutic efficacy.
Aaron Miller
October 21, 2025Honestly, if you’re not using fusidic acid for burns in this country, you’re missing the best topical antimicrobial, period, the evidence is overwhelming, the guidelines are crystal clear, and any deviation is just reckless, unpatriotic, and frankly, a mistake.
Roshin Ramakrishnan
October 22, 2025Hey everyone, just wanted to add that the global data supports its safety profile, and many burn centers worldwide have adopted it as a staple in their formulary, which shows how universally effective it really is! 😊
Todd Peeples
October 23, 2025From a pharmacokinetic standpoint, the molecule exhibits negligible systemic absorption, thereby minimizing hepatic first‑pass metabolism and renal clearance concerns; this facilitates its inclusion in multimodal regimens without necessitating dose adjustments. 📈
Leonard Greenhall
October 23, 2025The data presented aligns with the existing literature, though the sample size could be larger; still, the methodology appears sound and the conclusions are justified.
Abigail Brown
October 24, 2025When I first read about the new biogel matrix delivering fusidic acid over 48 hours, I felt a surge of hope that burn care could finally step into a more efficient era. Imagine a nurse spending half the time on dressing changes, freeing up resources for other critical patients. The early animal models showed not only faster re‑epithelialisation but also a surprising drop in bacterial counts, suggesting that sustained release may outmaneuver resistance mechanisms. This could mean fewer culture‑guided escalations to intravenous therapy, which is a game‑changer for both cost and patient comfort. Moreover, the biogel’s semi‑permeable nature maintains a moist wound environment, a cornerstone of optimal healing. Patients often report reduced pain scores when the dressing isn’t constantly being disturbed, which improves overall morale. From a microbiological perspective, the slow, steady diffusion keeps drug concentrations above the minimum inhibitory concentration for longer periods, a principle well‑known to pharmacologists but rarely achieved with traditional ointments. If clinical trials confirm these pre‑clinical findings, we may see a paradigm shift where topical therapy takes on a more prominent role even in moderately deep burns. The implications for antibiotic stewardship are profound; fewer systemic agents would translate to less disruption of the gut microbiome and lower rates of Clostridioides difficile infection. Additionally, hospitals could see a reduction in length‑of‑stay metrics, a critical quality indicator. The research team also hinted at the possibility of embedding other antimicrobial peptides into the matrix, opening doors for combinatorial approaches. Such innovation aligns perfectly with the push towards personalised, precision wound care. As clinicians, we’re always seeking tools that are both effective and easy to use, and this formulation seems to check both boxes. It’s exciting to think that in just a few years, the standard of care could include a single application that lasts two days, simplifying protocols dramatically. I’m eager to follow the upcoming phase‑II trial results, which promise to shed light on real‑world outcomes. Until then, the optimism surrounding this technology feels well‑earned, and I’m hopeful for the patients who will benefit.
Crystal Slininger
October 25, 2025While the data looks promising, one must consider the hidden influence of pharmaceutical lobbying on trial designs; the omission of long‑term resistance monitoring raises subtle red flags that are often glossed over in press releases.
Sumeet Kumar
October 26, 2025Thanks for the clear rundown – the stepwise approach makes it easy to teach residents, and the added note about pediatric safety is really valuable 😊.
Maribeth Cory
October 27, 2025Implementing this protocol now will raise our unit’s standard and show patients we’re proactive about infection control.
andrea mascarenas
October 27, 2025Good summary concise helpful
Vince D
October 28, 2025Agreed, the guidance is spot on.
Scott Swanson
October 29, 2025Oh sure, because adding more buzzwords to a simple ointment is exactly what we needed, right?