30 Oct 2025
- 10 Comments
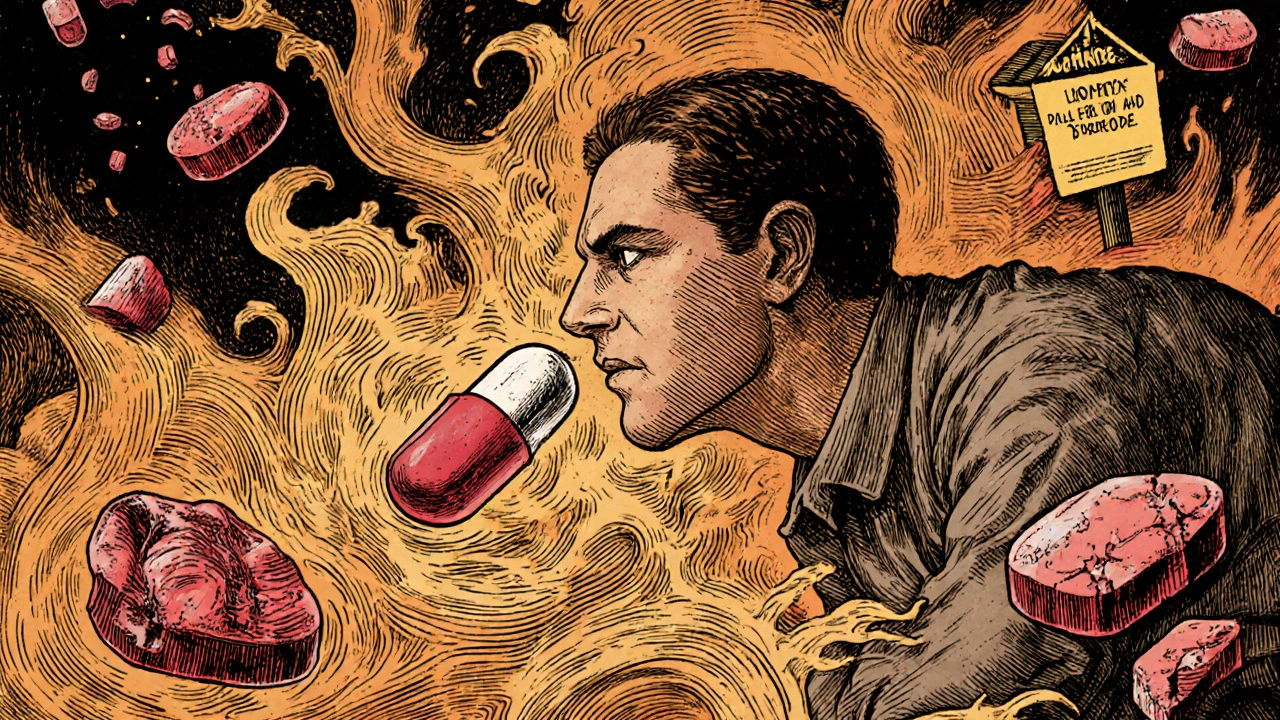
How Your Medication Gets Into Your Body Changes Everything
Think about the last time you took a pill. Maybe it was for a headache, an infection, or a chronic condition. You swallowed it without a second thought. But what if that same medicine, delivered in a different way, could cut your side effects in half? That’s not science fiction-it’s pharmacology. The way a drug enters your body-whether you swallow it, inject it, or rub it on your skin-determines not just how fast it works, but also what kind of trouble it might cause.
Oral: Convenient, But Hard on Your Gut
Oral meds are the default for a reason. They’re easy. You don’t need a needle. You don’t need help. About 75% of all prescriptions are taken by mouth. But that convenience comes with a cost. When you swallow a pill, it doesn’t just go straight to your bloodstream. It first has to survive stomach acid, get absorbed through your intestines, then pass through your liver-where up to 90% of some drugs get broken down before they even reach your system. This is called first-pass metabolism.
That’s why drugs like propranolol or penicillin V only work at 15-30% efficiency when taken orally. To make up for it, you get higher doses. And higher doses mean more side effects. About 25-30% of people on oral NSAIDs like ibuprofen or naproxen get stomach irritation. One in 50 long-term users ends up with a gastric ulcer. That’s not rare. That’s predictable.
And it’s not just your stomach. Food changes everything. Grapefruit juice can turn a safe dose of a cholesterol drug into a dangerous one. Antacids can block absorption of antibiotics. Forty percent of common oral medications interact with what you eat or drink. That’s why so many people stop taking them-not because they don’t work, but because they feel awful after taking them.
Injection: Fast, Precise, But Not Friendly
If speed matters, injections win. Give a painkiller intravenously, and it hits your brain in under five minutes. Give it orally? Thirty to ninety minutes. For emergencies-heart attacks, severe infections, anaphylaxis-injections are life-saving. They bypass your gut and liver entirely. That means 100% of the drug gets into your blood. No waste. No guesswork.
But here’s the catch: that precision comes with risk. One in five people who get intramuscular shots develop redness, swelling, or pain at the injection site. Needle phobia affects 1 in 5 adults. Some people freeze up, pass out, or avoid care altogether because of it. And it’s not just fear. Long-term users of insulin or biologics often develop lumps under the skin-lipohypertrophy-where repeated injections cause fat to build up. That messes up absorption, making doses unpredictable.
Cost is another barrier. A single monthly injection of a biologic drug can run $2,500 to $5,000. The oral version of the same drug? $25 to $100. Many patients skip doses or stop entirely because they can’t afford it. In one survey, nearly 30% of people on injectable medications admitted to skipping doses due to cost. That’s not noncompliance-it’s survival.

Topical: Localized Relief, Minimal Systemic Trouble
Topical treatments are the quiet heroes. Creams, gels, patches-these go straight where you need them. For eczema, arthritis pain, or muscle strains, applying medicine to the skin avoids your gut and liver almost entirely. Less than 10% of the active ingredient typically enters your bloodstream. That’s why topical corticosteroids cause 92% less HPA axis suppression than oral versions. That’s the difference between feeling fine and needing hormone replacement therapy.
Patients notice. On Drugs.com, topical pain relievers average 4.2 out of 5 stars. Oral versions? 3.7. Why? Because people say things like, “No nausea,” “No dizziness,” “No stomach pain.” Sixty-three percent of positive reviews for topical meds mention fewer side effects. That’s huge.
But topical isn’t perfect. Your skin isn’t a blank slate. If you have psoriasis or cracked skin, you might absorb 3 to 5 times more drug than intended. And if you don’t use enough? A 2022 study found that applying less than the recommended “fingertip unit” (about half a gram) cuts effectiveness by 40%. Most people don’t know how much to use. The instructions? Often printed in tiny font on a two-page insert. No wonder 60% of people apply topical meds incorrectly.
And then there’s the patch. Transdermal patches-like those for nicotine, fentanyl, or estrogen-deliver steady doses over hours. People with chronic pain love them because they avoid the highs and lows of oral meds. But 32% report skin irritation. And if you forget to remove it? You could overdose. That’s why patches come with warnings you rarely read.
Which Route Is Right for You?
There’s no universal best. It depends on what you’re treating, how fast you need relief, and what your body can handle.
Choose oral if:
- You need daily, long-term treatment for stable conditions (like high blood pressure or thyroid issues)
- You want the cheapest option
- You’re comfortable swallowing pills and can follow food rules
Choose injection if:
- You need immediate results (emergency, surgery, severe infection)
- Your gut can’t absorb meds (Crohn’s, vomiting, bowel obstruction)
- You’re in a hospital setting with trained staff
Choose topical if:
- You’re treating skin, joints, or localized pain
- You’ve had bad reactions to oral meds
- You want to avoid liver stress or GI issues

The Future Is Less Invasive
Pharma companies are racing to make injections obsolete. New tech is turning patches into smart delivery systems. Sontra Medical’s ultrasound-enhanced patch, approved in 2023, lets large molecules like proteins pass through skin-something once thought impossible. That means biologics, once only injectable, might soon be patchable. McKinsey predicts that by 2030, 25% of injectable drugs will shift to oral or topical forms.
Why? Because patients want control. They want fewer side effects. They want to avoid needles and stomach pain. And the data backs it up: when you reduce systemic exposure, you reduce harm.
But here’s the truth: not every drug can be moved. Thirty-seven essential medicines still require injection because they’re too big, too fragile, or too fast-acting to work any other way. That’s why we still need all three routes. The goal isn’t to eliminate injections-it’s to use the right one for the right person at the right time.
What You Can Do Today
Don’t just accept the side effects. Ask:
- Is there a topical version of this drug?
- Could I switch from oral to patch for steadier levels?
- Do I really need this injected, or could I take it by mouth?
Bring your pill bottle to your next appointment. Ask your pharmacist: “What’s the most common side effect with this, and is there a way to avoid it?” You’d be surprised how often they have a better option.
And if you’re using a topical cream? Use the right amount. A fingertip unit is not a smear. It’s a line from the tip of your finger to the first crease. That’s the dose. Too little? Waste. Too much? Risk.
Why do oral meds cause more stomach problems than injections or topicals?
Oral medications pass through your stomach and intestines, where they can irritate the lining. NSAIDs, for example, block protective enzymes in the gut, increasing the risk of ulcers. Injections and topicals bypass the digestive system entirely, so they don’t touch your stomach or intestines. That’s why people on oral painkillers often report nausea, heartburn, or bleeding-side effects you rarely see with patches or shots.
Can I switch from an injection to a pill if I hate needles?
Sometimes, yes-but not always. Many drugs, like insulin or certain biologics for autoimmune diseases, can’t be taken orally because the stomach breaks them down. But for conditions like osteoporosis or migraines, oral alternatives exist. Talk to your doctor: ask if a pill, patch, or nasal spray is available. Don’t assume you’re stuck with needles.
Are topical creams really as effective as pills?
For localized issues-like joint pain, eczema, or muscle soreness-yes, often more effective. A topical NSAID gel reduces inflammation right where it’s hurting, with almost no drug entering your bloodstream. An oral pill spreads the drug everywhere, which can cause side effects without adding benefit. But for systemic problems like high blood pressure or diabetes, topicals won’t work. The route must match the problem.
Why do some people get skin irritation from patches but not creams?
Patches often contain chemicals called permeation enhancers that force drugs through the skin. These can irritate sensitive skin. Creams usually have fewer additives and sit on top of the skin. Also, patches stay on for days, giving your skin no break. Creams are washed off. If you get redness from a patch, try rotating the site or switching to a cream version if available.
Is it safe to take more than the recommended dose of a topical cream if it’s not working?
No. Even though it’s applied to the skin, too much can still enter your bloodstream-especially if you have damaged skin, use it over large areas, or cover it with a bandage. For example, too much topical steroid can suppress your adrenal glands. Always follow the dose instructions. If it’s not working, see your doctor. Don’t guess.
Do injections always cause infections?
No. Infections at injection sites happen in only 1-5% of cases, and most are minor. The risk goes up if you reuse needles, don’t clean the skin, or have poor hygiene. Proper technique-sterile needle, clean skin, single use-makes infection extremely rare. Most people who get infections are either self-injecting incorrectly or using unsterile supplies.
Why are oral meds cheaper than injections?
Oral pills are easier and cheaper to make, store, and ship. They don’t need sterile packaging, syringes, or special handling. Injections require more complex manufacturing, cold chain logistics, and trained personnel to administer. That’s why a monthly oral pill might cost $50, while the same drug as an injection costs $2,500. Insurance often covers the pill but not the shot unless absolutely necessary.
Final Thought: It’s Not About the Drug-It’s About the Delivery
The medicine in your pill, shot, or cream is the same. But how it gets to your body? That changes everything. Side effects aren’t random. They’re predictable. They’re tied to the path the drug takes. The best treatment isn’t always the strongest. It’s the one that gets where it needs to go-with the least collateral damage.

Roy Scorer
October 31, 2025Let’s be real-pharma doesn’t care about your gut. They care about profit margins. Oral meds are cheaper to mass-produce, so they push them like candy. Meanwhile, your stomach lining turns into Swiss cheese and your liver throws a tantrum. They call it ‘compliance.’ I call it corporate abuse disguised as medicine.
Joseph Kiser
November 2, 2025You’re not alone in feeling this way. I’ve seen too many patients suffer needlessly because doctors default to pills without asking if there’s a gentler path. Topical options exist for so many conditions-and they’re *so* much kinder to the body. Don’t settle for ‘standard.’ Advocate for what works for YOU. 💪
Zachary Sargent
November 4, 2025Injection = needle terror. Oral = stomach hell. Topical = ‘why does this smell like chemical soup?’ No matter what, it’s a trade-off. I just want to feel better without becoming a science experiment.
Hazel Wolstenholme
November 5, 2025One must interrogate the epistemological foundations of pharmaceutical delivery paradigms. The hegemony of the oral route is not a biological imperative-it is a sociotechnical construct engineered by profit-driven institutions to maintain market dominance. The ‘fingertip unit’ is not a medical standard; it is a performative ritual of compliance. The skin, long dismissed as a passive barrier, is in fact a dynamic, semipermeable interface ripe for reclamation. Why are we still submitting to the tyranny of the pill?
Ajay Kumar
November 7, 2025Everyone’s talking about delivery methods like they’re the holy grail, but nobody’s talking about the fact that most of these drugs were designed in the 1950s for a world that didn’t have smartphones or AI. We’re still using century-old formulas and forcing them into modern bodies. And now we’re surprised people get side effects? Of course we do. The human body isn’t a vending machine that takes pills and spits out health. It’s a complex, evolving ecosystem. We treat it like a car that needs the right fuel-but we’re using diesel in a hybrid. The real solution isn’t patches or injections-it’s rethinking the drugs themselves. Stop patching the system. Redesign it.
Eileen Choudhury
November 8, 2025My grandma switched from oral ibuprofen to a topical gel for her arthritis-and suddenly she could hold her grandkids again without wincing. No stomach issues, no dizziness. Just relief. 🌿 It’s not magic, it’s science. And honestly? We need to celebrate these wins more. Small changes, big impact. You don’t always need a sledgehammer to fix a crack.
Mike Laska
November 9, 2025Wait-so you’re telling me that the reason I’ve been getting heartburn every time I take my blood pressure med isn’t just ‘bad luck’… it’s because my liver is literally eating it before it even gets to my blood? That’s insane. I’ve been blaming my coffee. Turns out, it’s the damn pill. I’m switching to a patch tomorrow. If I die, tell my cat I loved her.
Marcia Facundo
November 10, 2025I’ve been on oral meds for 12 years. I’ve had ulcers. I’ve cried in the bathroom. I’ve skipped doses because I couldn’t stomach the nausea. Then I found a patch. I don’t cry anymore. I don’t skip. I just… live. It’s not glamorous. But it’s mine.
Anthony Tong
November 11, 2025Topical? Patches? Please. This is the same nonsense the FDA pushes every decade. Next they’ll tell us to use crystals for diabetes. The only reason injections are expensive is because they’re regulated properly. Oral meds are sold like soda-unregulated, untested, and full of fillers. If you want safety, you pay for precision. If you want cheap, you get collateral damage. That’s capitalism. Accept it.
Alexa Apeli
November 13, 2025Thank you for this incredibly thoughtful and meticulously researched piece. 🌟 It’s rare to see such clarity on a topic so often muddled by misinformation. I’ve shared this with my entire family-and I’ve already scheduled a call with my pharmacist to discuss switching my migraine treatment to a transdermal option. Small steps, profound change. With gratitude and hope. 🙏