30 Apr 2023
- 13 Comments
Understanding Dry Mouth and Its Causes
Dry mouth, also known as xerostomia, is a common condition that occurs when the salivary glands in your mouth don't produce enough saliva to keep your mouth wet. Saliva plays a crucial role in maintaining a healthy oral environment, as it helps to keep our mouth clean, aids in digestion, and prevents infection. When there is a lack of saliva, you may experience a persistent dry feeling in your mouth, difficulty swallowing, and even bad breath.
There are various factors that can contribute to dry mouth. Some of the most common causes include medications, aging, dehydration, and certain medical conditions like diabetes, Sjogren's syndrome, and cancer treatments. It's essential to understand and address the underlying cause of your dry mouth to ensure you receive appropriate treatment and find relief.
What is Oral Thrush and Its Symptoms
Oral thrush, also known as oral candidiasis, is a fungal infection that occurs in the mouth. It is caused by an overgrowth of the Candida fungus, which is naturally present in our mouths. However, when the balance of microorganisms in the mouth is disrupted, Candida can multiply and cause an infection. This disruption can be due to various factors, including a weakened immune system, certain medications, and even dry mouth.
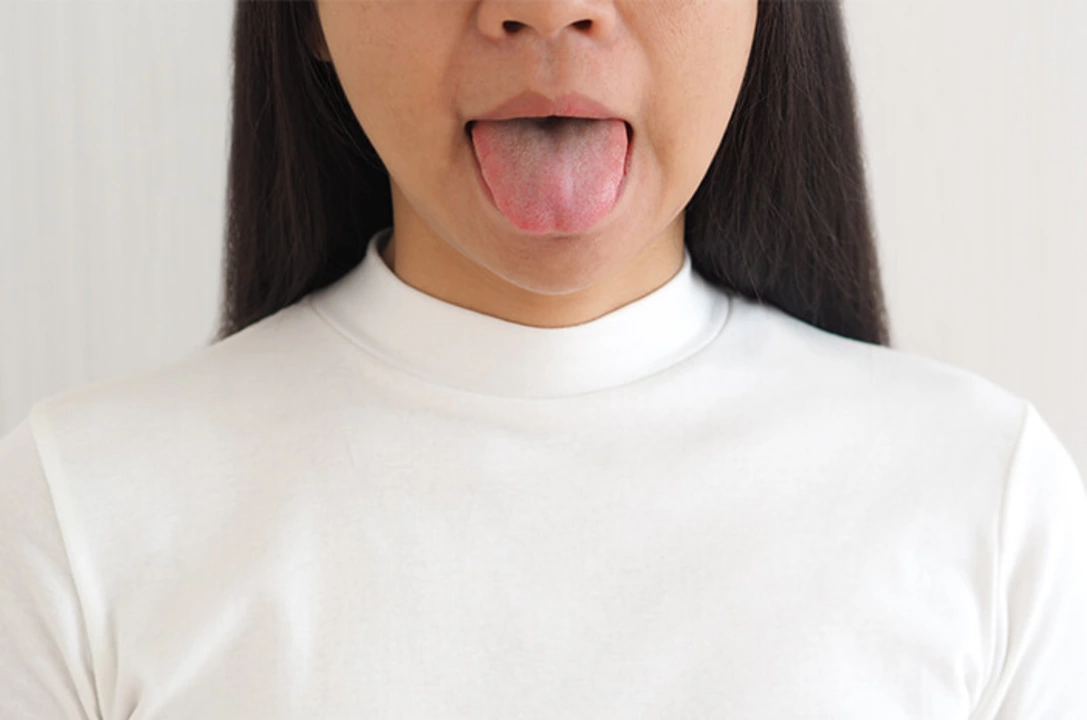
Oral thrush presents itself as white, creamy lesions on the tongue, inner cheeks, and sometimes the roof of the mouth, gums, and tonsils. Other symptoms may include a burning sensation in the mouth, a loss of taste, and difficulty swallowing. If left untreated, oral thrush can spread to other parts of the body and cause more severe health issues.
How Dry Mouth Contributes to Oral Thrush
As mentioned earlier, saliva plays a vital role in maintaining a healthy oral environment. One of its primary functions is to help control the growth of bacteria and fungi in the mouth. When there is a lack of saliva due to dry mouth, the balance of microorganisms in the mouth can be disrupted, allowing for the Candida fungus to multiply and cause oral thrush.
Moreover, dry mouth can also result from certain medications or medical conditions that can weaken the immune system. This weakened immune system can make it more difficult for your body to fight off infections, including oral thrush. Therefore, it's crucial to understand that dry mouth not only creates a favorable environment for Candida to thrive but can also be a contributing factor in weakening the immune system, making it easier for oral thrush to develop.
Preventing and Treating Dry Mouth and Oral Thrush
Preventing and treating dry mouth is essential in reducing the risk of oral thrush. Some steps you can take to manage dry mouth include staying hydrated, using a humidifier in your home, avoiding caffeine and alcohol, and chewing sugar-free gum to stimulate saliva production. Additionally, it's crucial to maintain good oral hygiene by brushing and flossing regularly and visiting your dentist for routine checkups.
If you suspect you have oral thrush, it's essential to see a healthcare professional for a proper diagnosis and treatment plan. Treatment for oral thrush typically involves antifungal medications, which can come in the form of lozenges, tablets, or liquid mouthwashes. In some cases, treating the underlying cause of the dry mouth can also help resolve the oral thrush infection.
When to Seek Professional Help
If you're experiencing persistent dry mouth or symptoms of oral thrush, it's essential to seek professional help as soon as possible. A healthcare professional can help determine the cause of your dry mouth and recommend appropriate treatment options. Additionally, they can diagnose and treat oral thrush, helping to alleviate your symptoms and prevent complications.
Remember, maintaining good oral hygiene and addressing dry mouth can significantly reduce your risk of developing oral thrush. Don't hesitate to reach out to a healthcare professional for guidance and support in managing these oral health issues.

Selena Justin
April 30, 2023Dealing with a dry mouth can be frustrating, especially when it starts affecting your taste and comfort. Staying hydrated throughout the day is a simple yet powerful tool, and sipping water regularly helps keep the oral cavity moist. Chewing sugar‑free gum or sucking on lozenges can stimulate saliva production without adding extra sugar. Pair that with a gentle oral rinse that’s alcohol‑free, and you’ll notice less irritation. Remember, a consistent oral hygiene routine-brushing, flossing, and regular dental check‑ups-supports both the gums and the natural defenses against thrush.
Bernard Lingcod
April 30, 2023Dry mouth isn’t just a nuisance; it can set the stage for fungal overgrowth if left unchecked. Incorporating a humidifier at night boosts ambient moisture and eases that parched feeling. Reducing caffeine and alcohol intake also removes two common culprits that dry out saliva glands. If you’re on medication, a quick chat with your doctor might reveal alternatives that are kinder to your mouth. Small lifestyle tweaks often make a big difference in keeping oral thrush at bay.
Raghav Suri
May 1, 2023Honestly, most people underestimate how much saliva protects you from opportunistic fungi. When you’re dehydrated, the balance tips in favor of Candida, and that’s when trouble starts. Boosting fluid intake isn’t just about quenching thirst; it’s a front‑line defense. And if you can’t drink more water, try electrolyte‑rich drinks that don’t contain sugar. Bottom line: keep that moisture engine running, or you’ll invite the bloom.
Freddy Torres
May 1, 2023Hydration is key.
Andrew McKinnon
May 2, 2023When your mouth feels like the Sahara, the fungus gets a free ride. Swapping to a saliva‑boosting gum can actually cut down on the white patches. Don’t forget to check if your meds are culprits-you might need a tweak. A quick visit to the dentist can spot early signs before they spread.
Dean Gill
May 2, 2023First and foremost, the body’s natural lubrication system is designed to keep pathogens at bay, so any disruption should be taken seriously. One practical step is to schedule regular water breaks, aiming for at least eight glasses a day, because even mild dehydration can reduce saliva output dramatically. Second, consider integrating a sugar‑free chewing gum or xylitol lozenge into your routine; these stimulate the parotid glands without adding fermentable carbs that feed candida. Third, assess your medication list-many antihistamines, antidepressants, and blood pressure drugs list xerostomia as a side effect, and a simple dosage adjustment or a switch to an alternative can restore normal flow. Fourth, explore non‑pharmacological aids like oral moisturizers, specifically those containing carboxymethylcellulose, which coat the mucosa and provide a protective barrier. Fifth, maintaining impeccable oral hygiene is non‑negotiable: brush twice daily with a fluoride toothpaste, floss regularly, and consider a chlorhexidine rinse if you’re prone to fungal growth. Sixth, dietary modifications matter; limit acidic and spicy foods that can further irritate a desiccated mouth and opt for soft, moist foods that don’t exacerbate dryness. Seventh, an occasional professional dental cleaning removes plaque biofilm that can harbor candida colonies, giving your immune system a clearer shot at control. Eighth, if home remedies fall short, consult your healthcare provider about prescription sialogogues like pilocarpine, which can pharmacologically stimulate salivary secretion. Ninth, for those with autoimmune conditions such as Sjögren’s syndrome, collaboration between a rheumatologist and dentist ensures a coordinated treatment plan targeting both systemic and oral manifestations. Tenth, remember that stress hormones can worsen xerostomia, so incorporating stress‑reduction techniques-mindfulness, yoga, or even short daily walks-can indirectly benefit salivary function. Eleventh, avoid alcohol‑based mouthwashes, which strip away the remaining moisture; opt instead for alcohol‑free formulations that soothe rather than dehydrate. Twelfth, during night-time, a humidifier can add ambient moisture, lessening the dryness that often intensifies while you sleep. Thirteenth, if you notice early signs of thrush-white patches, burning sensations, or altered taste-seek prompt medical attention; early antifungal intervention is far more effective than treating an entrenched infection. Fourteenth, keep a symptom diary; tracking triggers like specific foods, medications, or stress levels can help you pinpoint and eliminate the root causes. Finally, stay proactive and informed: the more you understand the interplay between saliva, oral flora, and systemic health, the better equipped you’ll be to prevent both dry mouth and its cascading complications.
Royberto Spencer
May 3, 2023It’s fascinating how often we accept dryness as an inevitable part of aging, yet it’s a clear invitation to microbial imbalance. By questioning the status quo and demanding a thorough evaluation, we empower ourselves to reclaim oral health. In the grand scheme, a dry mouth is a symptom, not a destiny, and addressing it reflects a broader philosophical commitment to bodily autonomy.
Annette van Dijk-Leek
May 4, 2023Absolutely love the proactive vibe here!!! Hydration + good hygiene = win!!! Keep those reminders coming!!!
Katherine M
May 4, 2023One must consider that the oral cavity, much like a micro‑cosmos, thrives on equilibrium. Disruption of salivary flow tilts this balance, allowing opportunistic fungi to proliferate. It is prudent, therefore, to adopt a regimen that safeguards moisture while preserving microbial diversity. 🌿
Bernard Leach
May 5, 2023Building on that, I’d suggest evaluating any underlying systemic conditions that might be diminishing salivary output, such as uncontrolled diabetes or medication side effects. Implementing a structured oral care schedule, perhaps using a timer, ensures consistency. In addition, exploring saliva substitutes containing natural mucopolysaccharides can provide a protective coating without altering the oral flora.
Shelby Larson
May 5, 2023People often ignore dry mouth until it becomes a full‑blown infection, which is just negligence. Proper oral care is a moral duty; ignoring it is essentially self‑harm. If you’re not proactive, you’re inviting preventable disease.
Mark Eaton
May 6, 2023Quick tip: keep a bottle of water at your desk and sip consistently; it’s a game‑changer for mouth dryness. Also, try a probiotic yogurt; the beneficial bacteria can help keep candida in check. Small habits add up to big results.
Alfred Benton
May 6, 2023It’s worth noting that many mainstream treatments overlook the subtle environmental factors that exacerbate xerostomia, possibly due to undisclosed industry influences. A thorough review of independent research reveals alternative protocols that are often suppressed. Therefore, a critical eye is essential when evaluating prescribed remedies.