SSRIs for PTSD: What Works, What Doesn’t, and What You Need to Know
When it comes to treating SSRIs for PTSD, selective serotonin reuptake inhibitors are a first-line medication option for managing trauma-related anxiety, depression, and hypervigilance. Also known as antidepressants for trauma, they don’t erase memories—but they help your brain handle them without falling apart. Unlike older drugs that just sedate you, SSRIs target the chemical imbalance linked to flashbacks, nightmares, and emotional numbness. The FDA has approved two: sertraline and paroxetine. But doctors often prescribe others like fluoxetine or escitalopram when those don’t work—or cause side effects.
It’s not magic. SSRIs for PTSD take weeks to kick in, and not everyone responds. Studies show about 60% of people see some improvement, but only about 20-30% get full symptom relief. That’s why they’re rarely used alone. Therapy like CBT or EMDR works better when paired with medication. And if you’re on birth control, have liver issues, or take other meds like NSAIDs or blood thinners, interactions matter. You can’t just pick one off the shelf. The right SSRI depends on your symptoms, other conditions, and how your body reacts to side effects like nausea, sleep changes, or sexual dysfunction.
Some people try SSRIs, feel worse at first, and quit too soon. That’s normal—initial anxiety spikes happen. But if you stick with it under a doctor’s watch, most side effects fade. Others find that one SSRI works wonders, while another makes them feel flat or disconnected. That’s why switching is common. Fluoxetine, for example, lasts longer in your system, so missed doses matter less. Sertraline tends to be gentler on the stomach. And paroxetine? It’s effective but can cause more weight gain and drowsiness. If you’ve tried one and it didn’t stick, it doesn’t mean they all won’t work.
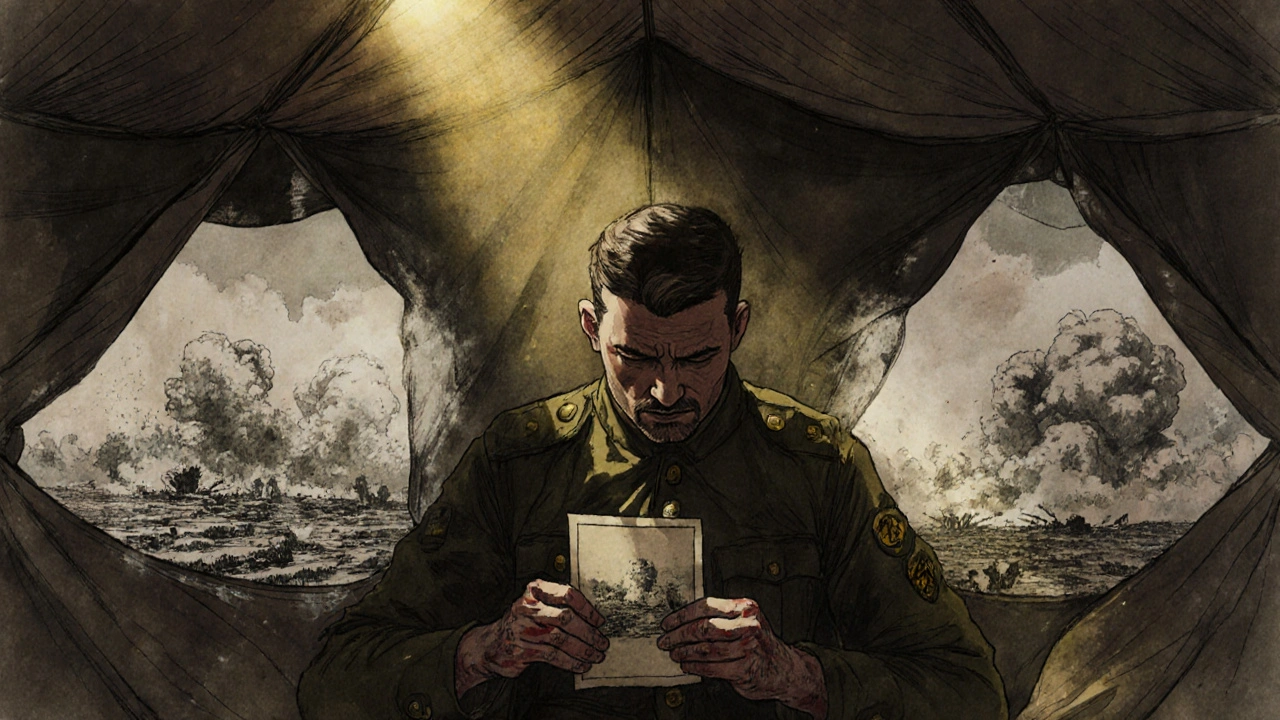
There’s no single answer. What works for a veteran with combat trauma might not help someone with childhood abuse. Your brain chemistry, life stress, and even your sleep habits change how SSRIs behave. That’s why the posts below cover real-world cases: how people managed side effects, what alternatives like SNRIs or prazosin helped when SSRIs failed, and how combining meds with therapy made the difference. You’ll find comparisons, patient experiences, and warnings about what not to mix with these drugs. This isn’t theory. It’s what people actually used—and what helped them get back on their feet.
Post-Traumatic Stress Disorder: How Trauma Processing and Medication Work Together
PTSD isn't just stress-it's a brain-based condition. Learn how trauma-focused therapy and medications like SSRIs and prazosin work, what actually helps, and why combining both may be the most effective path to recovery.