PTSD Treatment: Effective Therapies, Medications, and Real-Life Strategies
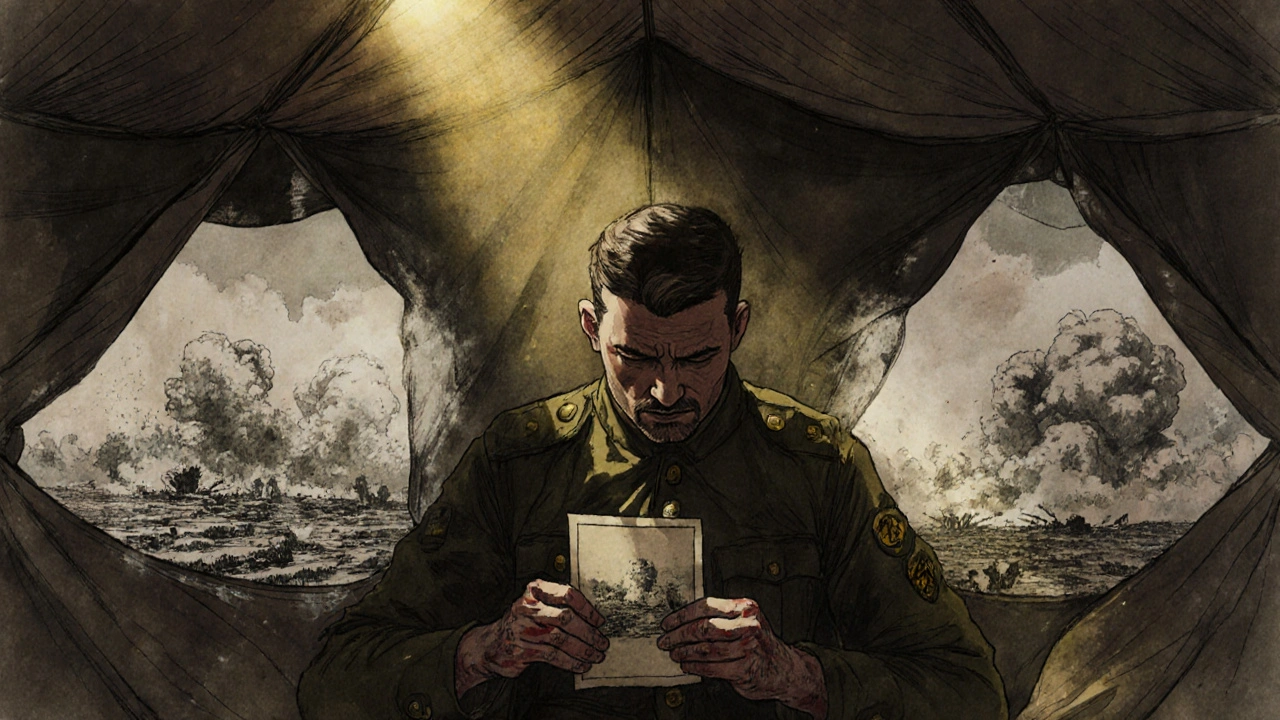
When someone lives with PTSD, a mental health condition triggered by experiencing or witnessing a traumatic event. Also known as post-traumatic stress disorder, it doesn’t just fade with time—it often needs active, targeted help to manage. Flashbacks, nightmares, hypervigilance, and emotional numbness aren’t just "bad days." They’re symptoms of a brain stuck in survival mode. And while it’s common to think PTSD only affects veterans, it shows up after car crashes, abuse, natural disasters, even sudden loss. The good news? PTSD treatment works—when it’s the right kind.
There are two main paths: therapy and medication. Cognitive Behavioral Therapy, a structured, goal-oriented talk therapy that helps reframe trauma-related thoughts is the gold standard. Specifically, Prolonged Exposure Therapy, a form of CBT where patients safely revisit trauma memories to reduce their power, has been shown in clinical trials to cut symptoms by 50% or more in just 10–15 sessions. Another effective approach is EMDR, Eye Movement Desensitization and Reprocessing, which uses guided eye movements to help the brain reprocess traumatic memories. These aren’t quick fixes—they’re rewiring tools. And they work better than pills alone.
Medications don’t cure PTSD, but they can make therapy possible. SSRIs, selective serotonin reuptake inhibitors like sertraline and paroxetine, are the only FDA-approved drugs for PTSD. They help with anxiety, depression, and sleep—side effects like nausea or sexual dysfunction are common, but often fade. Other meds, like prazosin for nightmares or mood stabilizers for anger, are used off-label when needed. But here’s the catch: meds without therapy often lead to relapse. The best results come from combining both.
What’s missing from most lists? Real-world support. Group therapy, peer networks, and even regular exercise can reduce cortisol levels and improve sleep. People who stick with treatment don’t just feel better—they start living again. They go back to work. They hug their kids without panic. They sleep through the night. The path isn’t linear, but it’s not impossible. Below, you’ll find real posts from people who’ve walked this road: what helped, what didn’t, and the hard truths about managing PTSD day after day.
Post-Traumatic Stress Disorder: How Trauma Processing and Medication Work Together
PTSD isn't just stress-it's a brain-based condition. Learn how trauma-focused therapy and medications like SSRIs and prazosin work, what actually helps, and why combining both may be the most effective path to recovery.