Prescription Medications: What You Need to Know About Safety, Interactions, and Use
When you take a prescription medication, a drug approved by health authorities for treating specific medical conditions under a doctor’s supervision. Also known as Rx drugs, these are not over-the-counter remedies—they’re powerful tools that require careful handling to avoid harm. Many people assume that because a doctor prescribed it, the medication is automatically safe. But prescription medications can cause serious side effects, dangerous interactions, or even life-threatening reactions if not used properly. This isn’t about fear—it’s about knowing what to watch for and how to take control.
One of the biggest risks comes from drug interactions, when two or more medications affect each other’s behavior in the body. For example, warfarin, a blood thinner used to prevent clots, can become dangerously strong when mixed with certain antibiotics, drugs used to fight bacterial infections. The same goes for levothyroxine, a thyroid hormone replacement, which loses effectiveness if taken with iron supplements, used to treat low iron levels. These aren’t rare cases—they happen every day, often because patients don’t know to ask.
Another hidden problem is medication adherence, how consistently a person takes their drugs as prescribed. Skipping doses, stopping early, or mixing pills with alcohol can turn a safe treatment into a health crisis. Think of it like charging a phone—you wouldn’t plug it in halfway and expect it to last all day. Yet millions do this with their meds. And for seniors managing five or more drugs at once, the risk of confusion, falls, or hospital visits skyrockets. That’s why deprescribing, the process of safely stopping unnecessary medications, is now a key part of modern care.
Then there’s the cost. Many assume brand-name drugs are better. But generic medications, chemically identical versions of brand-name drugs sold at lower prices, are often just as safe and effective. The FDA requires them to meet the same standards. Still, people hesitate—maybe they’ve heard stories of generics not working. Those cases are rare, but they happen when switching between different generic manufacturers. Knowing when to stick with one brand and when to switch can save hundreds a year without risking your health.
And let’s not forget how easily side effects get ignored. Muscle pain blamed on statins? Often not the drug. Insomnia from an antidepressant? Maybe it’s the timing. Constipation from opioids? Almost always, and there are proven fixes. The real issue isn’t the medication—it’s the lack of clear communication. Most people don’t know how to report bad reactions to the FDA, how to check if their online pharmacy is real, or even how to ask their doctor about alternatives. That’s why this collection exists: to give you the facts you won’t get in a 7-minute office visit.
Below, you’ll find real, practical guides on how to avoid dangerous mixes, track your pill schedule, spot counterfeit drugs, understand why your thyroid med isn’t working, and even how to talk to your doctor about cutting back. No fluff. No marketing. Just what works—and what doesn’t—based on clinical evidence and patient experience. Whether you’re managing a chronic condition, caring for an aging parent, or just trying not to get sick from your own meds, these posts will help you take smarter, safer steps.
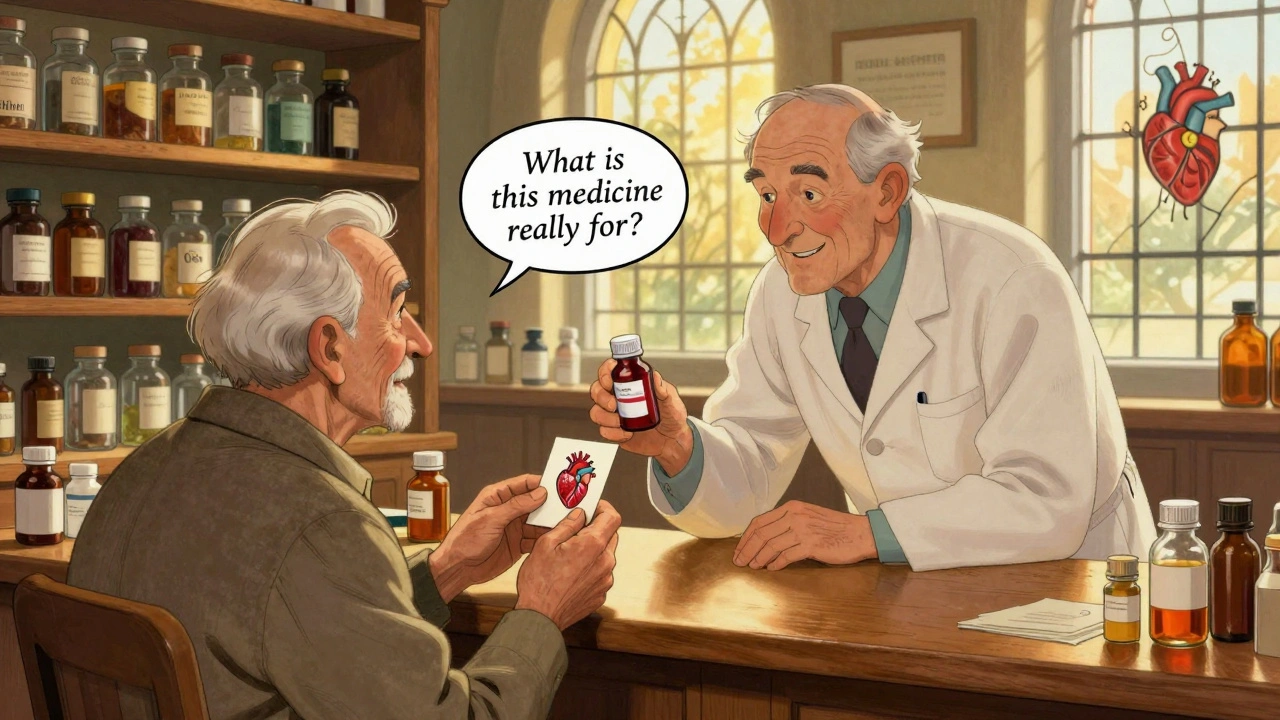
Questions to Ask Your Pharmacist About Prescription Medications
Knowing what to ask your pharmacist about your prescription meds can prevent dangerous interactions, reduce side effects, and save money. Learn the key questions to ask for safer, smarter medication use.