Menstrual Migraine
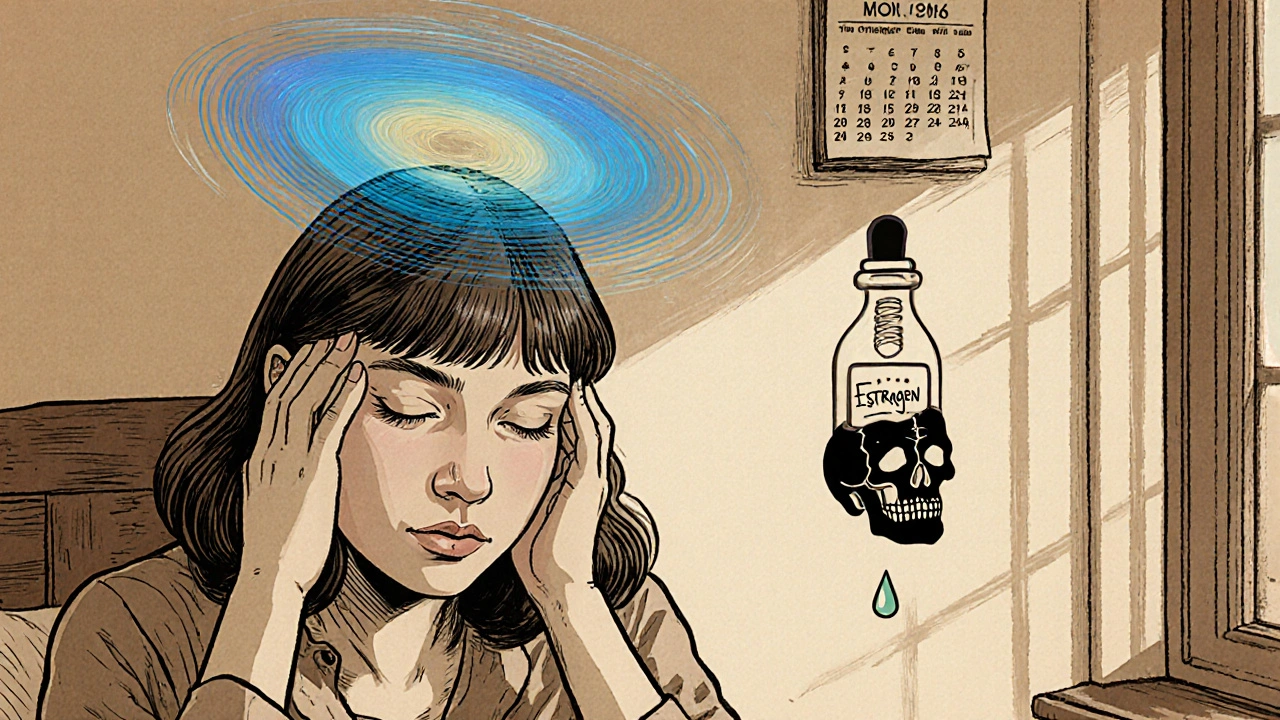
When dealing with menstrual migraine, the first step is to know what it actually is. Menstrual migraine, a type of headache that occurs in sync with a woman's menstrual cycle, typically during the days when estrogen levels fall. It’s also called hormonally triggered migraine. This condition isn’t just a bad day; it’s a pattern that shows up month after month, often catching sufferers off‑guard. Understanding the pattern helps you predict attacks and choose the right therapy.
Hormonal swing: estrogen and progesterone
The link between hormones and head pain is real. Estrogen, the primary female sex hormone that peaks mid‑cycle and drops sharply just before menstruation is the main driver. When estrogen plummets, blood vessels and brain chemicals react, sparking the migraine cascade. On the flip side, Progesterone, another cycle hormone that rises after ovulation and falls alongside estrogen can either dampen or amplify the pain, depending on individual sensitivity. These two hormones together shape the migraine window, so tracking their rise and fall gives you a roadmap for when attacks are most likely.
Because the hormonal trigger is clear, many doctors treat menstrual migraine by stabilizing hormone levels. Low‑dose estrogen patches or birth control pills that provide a steady hormone stream can blunt the dip that fuels the headache. Some patients prefer natural options like phytoestrogen‑rich foods or vitamin B6 supplements, which may smooth out the swing without a prescription. The key is to choose a method that matches your health profile and lifestyle, then stick with it long enough to see if the pattern changes.
Medication options: NSAIDs and triptans
When the hormonal approach isn’t enough, acute medication steps in. NSAIDs, non‑steroidal anti‑inflammatory drugs like ibuprofen or naproxen that reduce inflammation and block pain pathways are a first‑line choice because they target the prostaglandin surge that often accompanies menstrual bleeding. Taking an NSAID at the first sign of a headache can stop it before it fully develops. If NSAIDs don’t cut it, many turn to Triptans, serotonin receptor agonists such as sumatriptan that narrow blood vessels and halt migraine signaling. Triptans work especially well when the migraine has already kicked off, and they’re more effective if you’ve tried NSAIDs first and still have pain.
Choosing between NSAIDs and triptans often depends on how early you treat the attack, any other health conditions you have, and how your body responds. Some doctors recommend a “double‑hit” strategy: start with an NSAID as soon as the headache begins, then add a triptan if the pain persists after 30‑45 minutes. This layered approach can reduce the need for higher drug doses and lower the risk of side effects.
Tracking, lifestyle, and when to seek help
Beyond meds, lifestyle tweaks play a big role. Keep a simple headache diary that notes the day of your cycle, any stressors, diet changes, and medication taken. Patterns that emerge will confirm whether estrogen drops are truly the culprit or if other triggers—like caffeine, lack of sleep, or dehydration—are at play. Regular exercise, steady sleep schedules, and a diet low in processed sugars can blunt both hormonal and environmental triggers.
If your migraines are severe, last more than three days, or don’t improve with over‑the‑counter options, it’s time to see a specialist. Neurologists can run additional tests, adjust your hormonal regimen, or prescribe newer migraine‑specific drugs such as CGRP inhibitors. Early professional input often prevents the migraine from escalating into chronic daily headaches.
Below you’ll find a curated set of articles that dive deeper into each of these areas—from the science behind hormone fluctuations to step‑by‑step guides on using NSAIDs and triptans safely. Whether you’re looking for quick relief tips or a long‑term hormonal plan, the resources ahead will give you practical tools to manage menstrual migraine effectively.
Sumatriptan for Menstrual Migraines: Effectiveness, Dosage, and Risks
Explore how Sumatriptan can treat menstrual migraines, including its effectiveness, proper dosing, side‑effects, and alternative options for women seeking relief.