26 Apr 2023
- 19 Comments
Understanding Amiodarone and Its Use in Cardiac Resynchronization Therapy
As a copywriter, I've always been fascinated by the way medical advancements can improve our lives. One such advancement is the use of Amiodarone in Cardiac Resynchronization Therapy (CRT). In this section, we will explore what Amiodarone is, how it works, and why it has become such an important player in CRT.
Amiodarone is a medication used to treat various types of irregular heartbeats, or arrhythmias. It's classified as an antiarrhythmic drug, and it works by blocking certain electrical signals within the heart that can lead to an irregular heartbeat. By doing so, Amiodarone helps to restore a more regular and stable heart rhythm, allowing the heart to pump blood more efficiently.
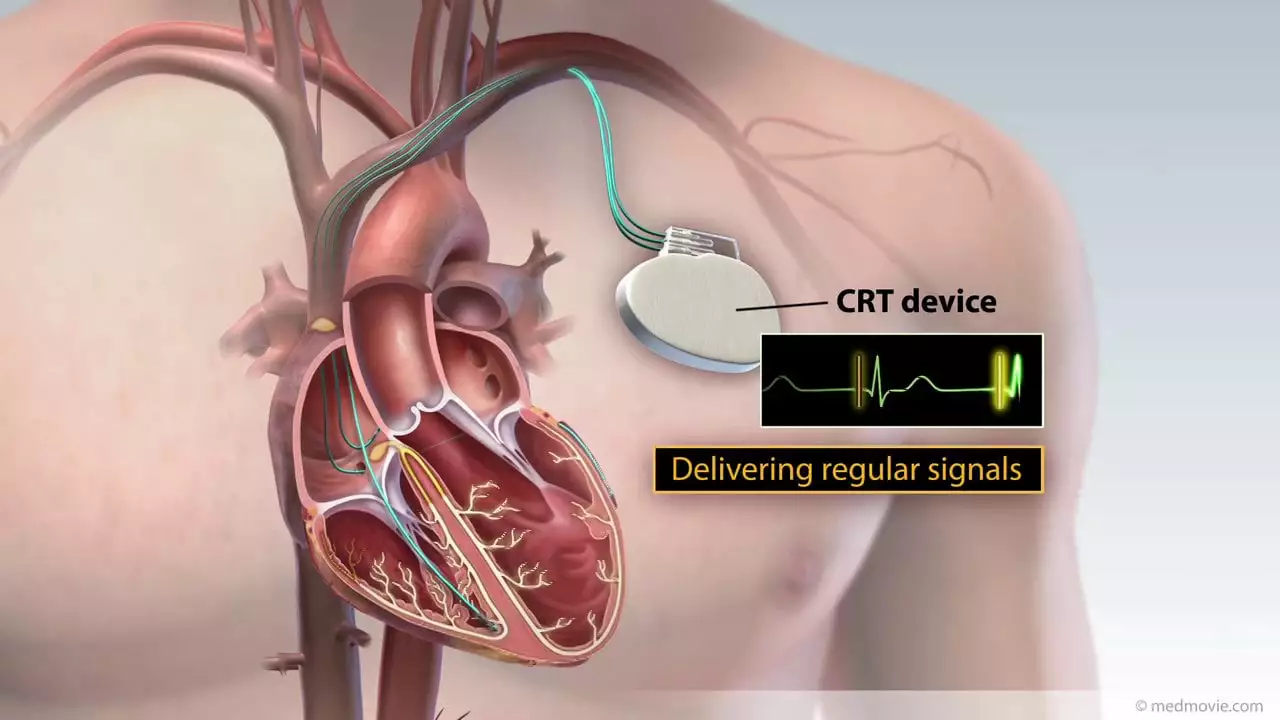
Cardiac Resynchronization Therapy is a treatment option for individuals who suffer from heart failure, particularly those who also experience ventricular dyssynchrony. This therapy involves the use of a specialized pacemaker that helps to coordinate the contractions of the heart's ventricles, improving the heart's overall function and reducing symptoms like shortness of breath and fatigue.
Now that we have a basic understanding of Amiodarone and CRT, let's delve deeper into the role that this powerful medication plays in this life-changing therapy.
The Benefits of Combining Amiodarone with CRT
When it comes to managing heart failure and arrhythmias, Amiodarone and CRT can be a powerful combination. The main reason for this is that Amiodarone can help to address some of the challenges that may arise during CRT, such as a persistent irregular heartbeat or the need for additional antiarrhythmic medications.
Studies have shown that adding Amiodarone to a CRT treatment plan can provide several benefits. For instance, patients who receive Amiodarone alongside CRT tend to experience fewer episodes of atrial fibrillation, a common type of arrhythmia. This, in turn, can help to reduce the risk of stroke, heart attack, and other complications associated with this condition.
Another key advantage of using Amiodarone in conjunction with CRT is that it may help to improve overall heart function. In some cases, patients who receive both therapies have been found to demonstrate significant improvements in their ejection fraction, which is a measure of how well the heart is pumping blood. This can lead to a better quality of life and a reduced need for hospitalization.
Overall, the combination of Amiodarone and CRT offers a promising approach to improving the lives of individuals with heart failure and arrhythmias, and it's exciting to see how this partnership is changing the landscape of cardiac care.
Identifying the Right Candidates for Amiodarone and CRT
As with any medical treatment, it's essential to determine which patients are the best candidates for Amiodarone and CRT. This process involves a thorough evaluation of the patient's medical history, current health status, and the severity of their heart failure symptoms. Some of the factors that may be considered when determining if a patient is a good candidate for this combined therapy include:
- The presence of ventricular dyssynchrony
- A history of atrial fibrillation or other arrhythmias
- Previous unsuccessful attempts to manage symptoms with other medications or treatments
- The existence of additional risk factors, such as advanced age or other chronic health conditions
By carefully assessing each patient's unique circumstances, medical professionals can make an informed decision about whether Amiodarone and CRT are the right course of action for their care.
Managing Potential Side Effects and Risks
As with any medication or medical intervention, there are potential side effects and risks associated with the use of Amiodarone and CRT. It's essential to be aware of these concerns to ensure that patients receive the most appropriate and effective care possible.
Some of the potential side effects of Amiodarone include dizziness, fatigue, nausea, and changes in vision. In rare cases, more severe complications such as liver or lung toxicity may occur. It's crucial for patients receiving Amiodarone to be closely monitored by their healthcare provider, and for any concerning side effects to be reported immediately.
Similarly, CRT carries its own set of risks, such as infection at the site of the pacemaker implant or potential malfunction of the device itself. As with Amiodarone, close monitoring and communication with healthcare providers are key to managing these concerns and ensuring the best possible outcome for the patient.
Monitoring Patient Progress and Adjusting Treatment Plans
As a patient undergoes treatment with Amiodarone and CRT, it's important for healthcare providers to closely monitor their progress and make any necessary adjustments to their treatment plan. This may include regular check-ups, blood tests, and imaging studies to evaluate the effectiveness of the therapies and identify any potential complications.
Based on the results of these evaluations, a patient's healthcare provider may make changes to their medication regimen or CRT settings, or they may recommend additional interventions, such as cardiac rehabilitation or lifestyle modifications, to further improve the patient's heart health and overall well-being.
Looking Ahead: The Future of Amiodarone and CRT
As medical research and technology continue to advance, it's exciting to consider the future of Amiodarone and CRT in the treatment of heart failure and arrhythmias. As we learn more about the best ways to combine these therapies and identify the patients who will benefit the most from their use, we can look forward to even better outcomes and quality of life improvements for those living with these challenging conditions.
As a copywriter, I'm honored to have the opportunity to share this information and bring awareness to the incredible advancements being made in the world of cardiac care. Together, we can continue to make strides in improving the lives of those affected by heart failure and arrhythmias, and look forward to a brighter future for all.

Jennifer Wees-Schkade
April 26, 2023Amiodarone's anti‑arrhythmic properties can dovetail nicely with CRT, especially when patients present with persistent atrial fibrillation. By stabilizing the cardiac rhythm, the device can achieve more synchronized ventricular contractions. Clinicians should evaluate liver and thyroid function before committing to long‑term therapy, as toxicity can undermine any pacing benefits.
Fr. Chuck Bradley
April 29, 2023One cannot help but feel a lingering sense of awe when contemplating the intricate dance between drug therapy and electrical modulation. The symphony of ion channels, pacemaker leads, and patient compliance creates a narrative that is both tragic and heroic.
Patrick Rauls
May 1, 2023Yo, if you're on Amiodarone and notice dizzy spells, don't just ignore'em – hit up your doc ASAP 😊. Also, keep an eye on those blood tests, they can spot liver issues before they become a nightmare.
Asia Lindsay
May 3, 2023Absolutely love seeing how CRT and Amiodarone can boost quality of life! 🌟 Remember, consistent follow‑ups are key – they keep the rhythm steady and the heart happy.
Angela Marie Hessenius
May 5, 2023When discussing the integration of Amiodarone into a cardiac resynchronization regimen, it is essential to first acknowledge the historical reluctance many clinicians have shown toward polypharmacy in heart failure patients. The early trials, which were hampered by small sample sizes and heterogeneous patient populations, painted a picture of limited benefit and heightened risk. Over time, however, subsequent multicenter studies have begun to paint a more nuanced portrait, revealing that specific subsets of patients actually thrive under combined therapy. In particular, those individuals who exhibit a high burden of ventricular ectopy and remain refractory to beta‑blockade appear to derive appreciable improvements in ejection fraction when Amiodarone is introduced alongside CRT. Moreover, the anti‑arrhythmic action of Amiodarone can mitigate the occurrence of atrial fibrillation episodes that would otherwise destabilize the synchronization achieved by the biventricular pacemaker. This reduction in arrhythmic burden not only lessens the symptomatology of palpitations and dyspnea but also translates into a lower incidence of hospitalization for heart‑failure exacerbations. Clinicians must, however, remain vigilant regarding the drug’s known side‑effect profile, including potential pulmonary fibrosis, thyroid dysfunction, and hepatic enzyme elevations. Regular monitoring protocols, involving quarterly liver function tests, biannual thyroid panels, and annual high‑resolution chest imaging, are therefore indispensable components of comprehensive care. Patient education plays an equally pivotal role; individuals need to understand the importance of reporting new visual disturbances or unexplained skin changes promptly. From a mechanistic standpoint, Amiodarone’s class III properties prolong the action potential duration, a phenomenon that harmonizes well with the paced ventricular depolarization achieved through CRT. Yet, this same effect can predispose to torsades de pointes if electrolyte imbalances are not corrected, underscoring the necessity of meticulous electrolyte management. If these considerations are judiciously addressed, the synergistic effect of Amiodarone and CRT can be harnessed to produce a measurable increase in functional capacity, often reflected in higher six‑minute walk test distances. Additionally, patients frequently report an enhanced sense of well‑being, which can be attributed to the reduced frequency of symptomatic arrhythmias. The economic implications are also worth noting; by decreasing rehospitalization rates, combined therapy may ultimately reduce healthcare expenditures. In conclusion, the evolving evidence base supports a tailored approach: not every CRT recipient requires Amiodarone, but for those with refractory arrhythmias, the benefits frequently outweigh the risks.
Julian Macintyre
May 6, 2023It must be observed that the aforementioned exposition suffers from a paucity of rigorous statistical substantiation. While the anecdotal benefits of Amiodarone co‑administration are extolled, the author neglects to delineate confidence intervals, p‑values, or the sample sizes underpinning cited studies. Moreover, the potential for iatrogenic complications, particularly pulmonary toxicity, is relegated to a cursory mention, an omission that could mislead practitioners seeking a balanced appraisal. A more methodical synthesis, incorporating meta‑analytic data, would enhance the credibility of the discourse.
Patrick Hendrick
May 8, 2023Indeed, the interplay of pharmacology and device therapy, while complex, offers tangible benefit, provided clinicians adhere to stringent monitoring protocols, maintain dosage vigilance, and engage patients in shared decision‑making.
abhishek agarwal
May 10, 2023Look, if you think adding another drug to an already sick heart is a bad idea, you’re missing the point – Amiodarone fixes the rhythm mess, lets the CRT actually do its job, and that’s a win for everyone.
Michael J Ryan
May 11, 2023i totally get where you're coming from, but i think it's also key to balance the pros with the cons, especially when dealing with long‑term side effects like thyroid issues.
Khalil BB
May 12, 2023Sure, but the rhythm control wins outweigh the thyroid risk when you monitor labs regularly.
Keri Shrable
May 15, 2023Amiodarone can really smooth out CRT performance.
Destiny Hixon
May 17, 2023Honestly, anyone who doubts this combo is just following foreign pharma hype, stay strong and trust the US guidelines.
mike brown
May 18, 2023Well, that’s just another echo chamber; I’d rather see hard data before buying into the hype.
shawn micheal
May 20, 2023There's a lot of optimism hanging around this therapy, and honestly I think that’s justified. When patients finally feel less short‑of‑breath, they regain confidence in daily activities, which can cascade into better adherence overall. The psychological boost from seeing improvement shouldn't be underestimated – it’s part of healing too. So, with proper oversight, this partnership between drug and device holds real promise.
Stephen Jahl
May 21, 2023From a hemodynamic perspective, the synergistic modulation of atrioventricular synchrony via biventricular pacing, concomitant with class III anti‑arrhythmic pharmacodynamics, yields a reduction in intracavitary pressure gradients that is quantifiable through invasive catheterization metrics.
gershwin mkhatshwa
May 24, 2023Sounds like a solid combo – just keep an eye on those side‑effects and stay in touch with your EP team.
Louis Robert
May 25, 2023Monitoring is key.
tim jeurissen
May 27, 2023While the author’s enthusiasm is commendable, the prose would benefit from the eradication of colloquialisms, the insertion of precise lexical choices, and the strict adherence to syntactic parallelism throughout the manuscript.
lorna Rickwood
May 29, 2023Life beats in rhytm, and the heart finds its song when tech and med unite, dont you think?